The U.S. healthcare system runs on generics. Nine out of every ten prescriptions filled today are for generic drugs - not because they’re second-rate, but because they’re just as safe and effective as the brand-name versions, and they cost up to 85% less. But how does the FDA make that possible? The answer lies in a 40-year-old law, a streamlined approval process, and a system designed to balance innovation with affordability. This isn’t guesswork. It’s science, regulation, and legal structure working together - and it’s what keeps millions of Americans able to afford their medicines.
The Legal Foundation: The Hatch-Waxman Act
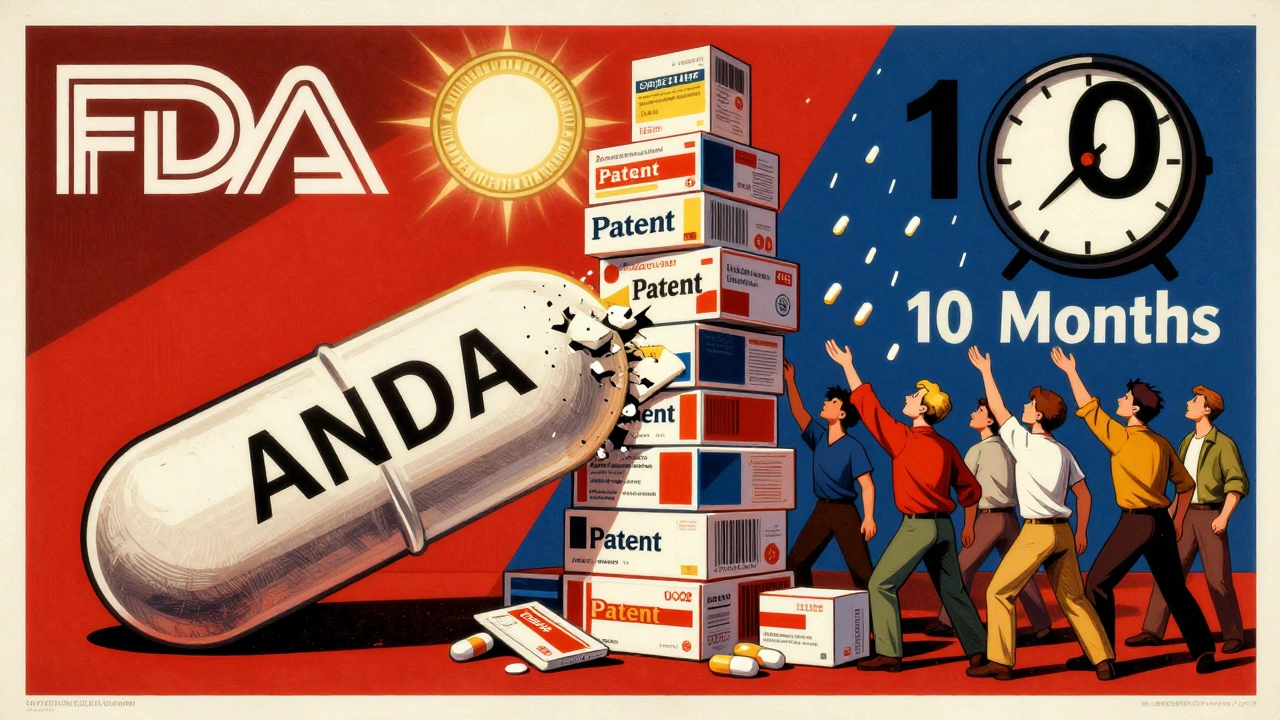
The entire system of generic drug approval in the U.S. traces back to one law: the Drug Price Competition and Patent Term Restoration Act of 1984, better known as the Hatch-Waxman Act. Before this law, generic manufacturers had to repeat every clinical trial done by the original drugmaker - a costly, time-consuming process that made generic versions economically unfeasible. Hatch-Waxman changed that. It created the Abbreviated New Drug Application (ANDA) pathway under Section 505(j) of the Federal Food, Drug, and Cosmetic Act. This meant generic companies no longer needed to prove a drug was safe and effective from scratch. Instead, they could rely on the FDA’s prior findings for the brand-name drug, called the Reference Listed Drug (RLD).The law didn’t just lower costs - it created a legal framework for competition. It gave brand-name companies a limited period of market exclusivity (up to five years for new chemical entities) while also giving the first generic applicant a 180-day exclusivity window if they successfully challenged a patent. This balance encouraged innovation without blocking access to cheaper alternatives. Today, the ANDA pathway is the backbone of the U.S. generic drug market, which saved the healthcare system over $370 billion in 2023 alone.
What the FDA Actually Requires for Approval
Getting FDA approval for a generic drug isn’t easy - it’s just different from the brand-name process. The FDA doesn’t cut corners. It demands exact matches in key areas:- Active ingredient: Must be identical in chemical structure and concentration.
- Strength and dosage form: Same tablet size, capsule, injection, or inhaler as the brand.
- Route of administration: Oral, topical, IV - must match exactly.
- Use indications: Approved for the same medical conditions.
- Manufacturing standards: Produced in facilities that meet the same Good Manufacturing Practice (GMP) rules as brand-name plants.
The most critical requirement is bioequivalence. A generic drug must deliver the same amount of active ingredient into the bloodstream at the same rate as the brand drug. This is tested in 24 to 36 healthy volunteers using pharmacokinetic studies. Blood samples are taken over hours to measure how quickly the drug is absorbed and how long it stays in the body. The FDA requires the generic’s absorption rate to fall within 80% to 125% of the brand’s - a tight range that ensures clinical equivalence.
It’s not enough to have the same pill. The inactive ingredients - like fillers, dyes, or preservatives - can differ. But those can’t affect how the drug works. If a dye causes an allergic reaction in a small number of people, the generic must still be safe for everyone else. The FDA reviews every component.
The ANDA Submission and Review Process
Submitting an ANDA is a complex, multi-step process. It starts with a Filing Review. The FDA checks if the application is complete: Are all required sections included? Is the chemistry data solid? Is the manufacturing facility registered? If something’s missing - say, a missing stability study or an unapproved facility - the FDA issues a Refuse-to-Receive (RTR) letter. No review happens. The company must fix the issue and pay a new filing fee.Once filed, the application moves to substantive review under the Generic Drug User Fee Amendments (GDUFA). This program, first launched in 2012 and renewed through GDUFA III in 2022, gives the FDA funding to hire more reviewers and set clear timelines. For a standard ANDA, the FDA aims to complete its review within 10 months. For priority applications - like drugs in short supply or first-time generics - the goal is 8 months. This is a major improvement from the pre-GDUFA era, when reviews could drag on for years.
During review, the FDA examines every part of the application: Chemistry, Manufacturing, and Controls (CMC) data; bioequivalence study protocols; proposed labeling; and facility inspection reports. The agency may inspect the manufacturing site - even if it’s overseas - to verify compliance with U.S. standards. In 2023, the FDA approved 90 first-time generic drugs, down from 107 in 2022, reflecting tighter scrutiny and more complex submissions.

Patents, Exclusivity, and Legal Hurdles
One of the most complicated parts of getting a generic to market isn’t science - it’s law. Brand-name companies list their patents in the FDA’s Orange Book. Generic applicants must certify how they’ll handle those patents. There are four types of certifications, but the most contentious is the Paragraph IV certification: a legal challenge claiming the patent is invalid or won’t be infringed.If a brand-name company sues within 45 days of receiving that notice, the FDA is automatically blocked from approving the generic for 30 months - unless a court rules in favor of the generic maker sooner. This is called the 30-month stay. It’s a powerful tool. Some brand companies file dozens of weak patents - a practice called “patent thickets” - to delay competition. The FDA can’t override these lawsuits. It can only wait.
On the flip side, the first generic company to file a successful Paragraph IV certification gets 180 days of market exclusivity. No other generic can enter during that time. This creates a rush to file - and sometimes, legal battles over who qualifies as the “first.”
Complex Generics and Emerging Challenges
Not all drugs are created equal. Simple pills - like metformin or lisinopril - are easy to copy. But what about inhalers, injectable gels, or extended-release patches? These are called complex generics. Their effectiveness depends not just on the active ingredient, but on how the drug is delivered. A generic inhaler must match the spray pattern, particle size, and lung deposition of the brand. That’s not something bioequivalence studies alone can prove.The FDA has acknowledged this gap. In 2023, it launched the Complex Generic Drug Product Development Resources initiative to provide guidance and scientific support to manufacturers. The goal? To reduce the number of failed applications and speed up approvals for these harder-to-copy drugs. In October 2025, the FDA announced a new pilot program that prioritizes ANDA reviews for companies that test and manufacture their products in the U.S. - a direct response to supply chain concerns.

Who Benefits? And Who’s Left Behind?
Patients benefit the most. Generic drugs are the reason millions can afford insulin, blood pressure meds, and antidepressants. Providers benefit too - fewer patients skip doses because of cost. The system has saved the U.S. healthcare system hundreds of billions over the past decade.But it’s not perfect. Some patients report subtle differences in how a generic feels - though the FDA says these are rarely clinically meaningful. Others face delays because of patent litigation or manufacturing issues. And while big players like Teva, Sandoz, and Viatris dominate the market, smaller companies struggle with the cost and complexity of ANDA submissions. The FDA’s focus on faster reviews and domestic manufacturing is a step toward fixing that.
The real test comes with next-generation drugs. As more treatments become biologics - complex proteins made from living cells - the ANDA pathway won’t work. That’s where biosimilars come in, under a separate law called the BPCIA. But for now, the ANDA system remains the gold standard for small-molecule generics. It’s not glamorous. But it works.
Are generic drugs really as effective as brand-name drugs?
Yes. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also demonstrate bioequivalence - meaning they deliver the same amount of drug into the bloodstream at the same rate. Thousands of studies and decades of real-world use confirm that generics work just as well. The FDA monitors adverse events for both brand and generic drugs and finds no consistent difference in safety or effectiveness.
Why do some generics look different from the brand name?
U.S. law requires generics to look different from brand-name drugs to avoid trademark infringement. That means the color, shape, or imprint on the pill can change. But these differences are only in inactive ingredients - like dyes or binders - which don’t affect how the drug works. The active ingredient is identical. If you’re concerned about a change in appearance, talk to your pharmacist - but don’t assume it affects effectiveness.
How long does it take for the FDA to approve a generic drug?
Under current GDUFA guidelines, the FDA aims to complete its review of a standard ANDA within 10 months of submission. For priority applications - such as drugs in short supply or first-time generics - the goal is 8 months. This is a significant improvement from the 1980s, when reviews could take years. Timelines can be extended if the application is incomplete or if the FDA requests additional data.
Can a generic drug be pulled from the market after approval?
Yes. The FDA can withdraw approval if a generic manufacturer fails to maintain quality standards, misrepresents data, or if post-market safety issues arise. The agency conducts routine inspections of manufacturing sites and monitors adverse event reports. In 2023, the FDA revoked approval for several generic versions of a popular blood pressure medication after testing found inconsistent potency levels. The system isn’t perfect, but it has checks in place.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs made through chemical synthesis - like aspirin or metformin. Biosimilars are highly similar versions of complex biological drugs - like insulin or Humira - made from living cells. Because biological drugs are inherently more variable, biosimilars don’t have to be identical, just highly similar with no clinically meaningful differences. They’re approved under a different law (BPCIA) and require more extensive testing than traditional generics.
What Comes Next?
The FDA’s focus is shifting. With drug shortages still a problem and complex generics harder to replicate, the agency is pushing for more domestic manufacturing and better tools to evaluate advanced drug forms. The new pilot program for U.S.-based manufacturers signals a policy shift - one that ties faster approvals to local production. Meanwhile, research continues into how to better assess complex delivery systems like transdermal patches and inhalers.The system isn’t broken. It’s working - just not perfectly. The Hatch-Waxman Act created a framework that brought affordable medicine to millions. The challenge now is adapting it for the next 40 years. That means smarter regulation, more transparency, and a commitment to keeping generics not just legal - but reliable, accessible, and always safe.

Lynette Myles
December 4, 2025 AT 18:05The FDA approves generics based on bioequivalence studies with 24 volunteers? That’s not science - it’s a gamble. What about long-term effects? What about drug interactions over years? They don’t test that. They just assume. And we’re supposed to trust this?
My uncle died on a generic blood thinner. The brand worked. The generic didn’t. They said it was ‘within 80-125%’ - that’s a 45% window. That’s not a match. That’s a lottery.
They call it science. I call it corporate convenience dressed in lab coats.
Annie Grajewski
December 4, 2025 AT 20:55so like… the fda just says ‘eh, close enough’ and we all live happily ever after? lol. i mean, i get it, cheaper meds = less bankruptcy, but also… what if my body just hates the dye in the generic version of my antidepressant? i switched and felt like a zombie for 3 weeks. no one told me the ‘inactive ingredients’ could make me want to cry into my cereal.
also who decided ‘80-125%’ was chill? that’s like saying your pizza is ‘close enough’ if it’s 20% pineapple or 25% shoe leather. 🤡
Jimmy Jude
December 6, 2025 AT 18:30Let’s be real - this whole system is a theater of illusions. We’re told generics are ‘just as good’ - but what does ‘good’ even mean? Is it the pill that fits in your hand? Or the one that doesn’t make you feel like your soul is being slowly siphoned out through your kidneys?
The FDA doesn’t care about your experience. They care about data points. And data points don’t feel panic attacks at 3 a.m. because your anxiety med ‘wasn’t quite right’ this week.
They’re not saving lives. They’re optimizing spreadsheets.
Rupa DasGupta
December 8, 2025 AT 00:43OMG I can't believe this!!! 😭 I switched to generic metformin and my blood sugar went CRAZY. Like, I had to go to the ER. And they just said 'it's bioequivalent' like that fixes everything??
My grandma in India takes the same drug from a local pharma and she's fine. Why can't we have that here? Why do we have to pay for corporate drama?? 😤
ashlie perry
December 9, 2025 AT 15:02They don’t test for long-term. They don’t test for you. They test for the average. You’re not average. You’re the one who gets sick because the filler in the generic gives you migraines. And they don’t care.
It’s legal. That’s all that matters.
Juliet Morgan
December 10, 2025 AT 00:56I just want to say - if you’re struggling with the cost of meds, please know you’re not alone. I’ve been there. Switching to generics saved my life. I didn’t feel any difference. And I know some people do - that’s real too.
But please don’t give up. Talk to your pharmacist. Ask for samples. There are patient assistance programs. You deserve to feel better. I believe in you 💪❤️
Katie Allan
December 10, 2025 AT 06:08The Hatch-Waxman Act was a quiet revolution. It didn’t make headlines, but it turned medicine from a luxury into a right. For millions, it meant choosing between insulin and groceries - and now, it means choosing between two brands of insulin, both affordable.
Yes, the system has flaws. But dismantling it won’t fix them. We need better oversight, not less access. The goal isn’t perfection - it’s justice. And this law delivered that, imperfectly, but meaningfully.
Deborah Jacobs
December 12, 2025 AT 05:26Generics are the unsung heroes of American healthcare. No one throws parades for them. No one sings songs about the guy who made the generic version of lisinopril. But every morning, millions swallow those little pills and live another day - because someone, somewhere, fought to make them cheap enough to afford.
It’s not magic. It’s chemistry. It’s regulation. It’s grit. And yeah, sometimes it fails. But mostly? It works. And that’s worth defending.
Krishan Patel
December 12, 2025 AT 10:30This entire system is a betrayal of the public trust. The FDA is not a guardian - it is a pawn of Big Pharma. The 180-day exclusivity window? A backdoor monopoly. The Paragraph IV certifications? A legal loophole designed to enrich law firms, not patients.
And now they want to reward U.S.-based manufacturers? What about the global South? Are we supposed to believe that only American factories can be trusted? This is economic nationalism dressed as public health.
Carole Nkosi
December 13, 2025 AT 10:40They say generics are safe. But I’ve seen what happens when you cut corners. My cousin got kidney damage from a generic antibiotic. The company didn’t even have a GMP certificate. The FDA approved it anyway. Because they were behind on deadlines.
This isn’t regulation. It’s negligence with a stamp.
Manish Shankar
December 14, 2025 AT 20:07It is imperative to acknowledge the structural integrity of the Abbreviated New Drug Application pathway as a cornerstone of pharmaceutical accessibility. The bioequivalence threshold of 80–125% is not arbitrary; it is statistically validated through rigorous pharmacokinetic modeling and peer-reviewed clinical methodology. To dismiss this framework without empirical counter-evidence constitutes a fundamental misunderstanding of pharmacological science.
luke newton
December 14, 2025 AT 22:12Oh please. You think the FDA gives a damn about you? They’re owned by the same pharma giants that make the brand-name drugs. The ‘first generic’ gets 180 days? That’s not competition - that’s a pay-to-play scheme.
And don’t even get me started on overseas factories. You think your ‘safe’ generic was made in a clean U.S. lab? Nah. It was made in a basement in Bangalore with a guy named Raj who doesn’t speak English.
And you’re still swallowing it? Pathetic.
an mo
December 16, 2025 AT 09:57Let’s cut the fluff. The ANDA system is a national security vulnerability. We’re dependent on foreign manufacturing for 80% of our active pharmaceutical ingredients. China and India control the supply chain. The FDA’s ‘review timelines’ are theater. What’s really happening is a silent erosion of our medical sovereignty.
And now they want to incentivize domestic production? Too little, too late. We should have nationalized the supply chain 20 years ago. Now we’re one pandemic away from mass death by pill shortage.
Marvin Gordon
December 17, 2025 AT 15:20Man, I used to be scared of generics. Thought they were ‘cheap knockoffs.’ Then I got on a $4 prescription plan and tried the generic for my cholesterol med. Same results. Same no side effects. Saved me $200 a month.
Yeah, some people have weird reactions - that’s real. But for most of us? It’s just the same pill with a different color.
Don’t fear the generic. Fear the price tag. That’s the real enemy.
Norene Fulwiler
December 18, 2025 AT 19:43In my village in Mexico, we’ve been using Indian generics for years. No one dies. No one gets sick. We don’t have brand-name drugs because we can’t afford them. But we live. We take our meds. We go to work.
The FDA’s standards are good. But they’re not the only way. Maybe we need to stop assuming that American rules = universal truth.
There’s dignity in affordability.