H1 vs H2 Blocker Selector
Select your symptoms to determine whether you need H1 blockers (for allergies) or H2 blockers (for stomach acid issues). This tool is for educational purposes only and does not replace medical advice.
Allergy Symptoms
Stomach Acid Symptoms
Most people know antihistamines for allergy relief, but not everyone realizes there are two main types with very different uses: H1 blockers and H2 blockers. They sound similar, but they work in completely different parts of your body and come with very different side effects. Mixing them up can lead to wasted money, unnecessary drowsiness, or even missed treatment for something like heartburn.
What H1 Blockers Actually Do
H1 blockers target histamine receptors in your skin, nose, lungs, and blood vessels. These are the spots where your body reacts to allergens like pollen, pet dander, or dust mites. When histamine binds there, you get sneezing, itching, runny nose, and hives. H1 blockers stop that reaction before it starts.
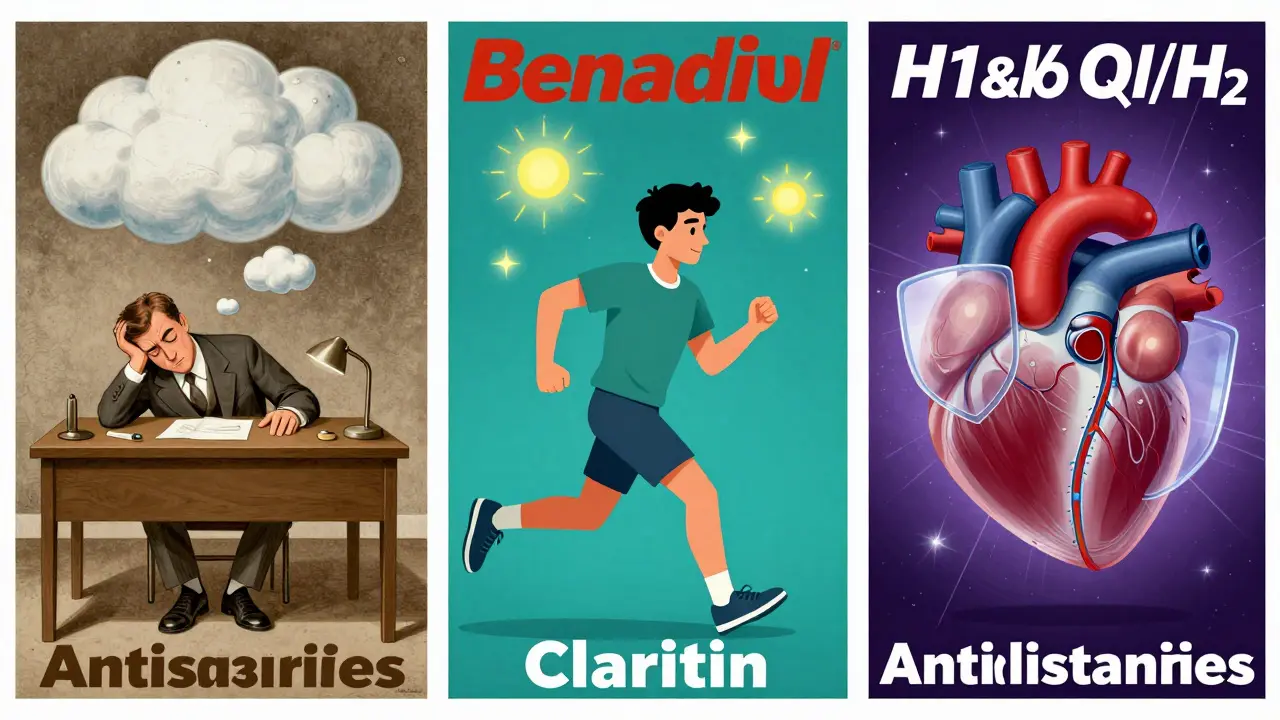
The first ones, like diphenhydramine (Benadryl), came out in the 1940s. They work fast-often in under 30 minutes-but they cross into your brain. That’s why so many people feel sleepy after taking them. Studies show 30 to 50% of users report drowsiness. That’s not just a side effect-it’s a safety issue. Older adults are at higher risk of falls, confusion, and memory problems. The American Geriatrics Society specifically warns against using these in people over 65.
Today, most people use second- or third-generation H1 blockers like loratadine (Claritin), fexofenadine (Allegra), or cetirizine (Zyrtec). These were designed to stay out of the brain. They cause drowsiness in only 10 to 15% of users. That’s why they’re the go-to for daily allergy management. You can take them once a day, no matter the time, and still drive, work, or care for kids without feeling wiped out.
What H2 Blockers Actually Do
H2 blockers don’t touch your allergies. They go straight to your stomach. That’s where histamine signals acid-producing cells to release gastric acid. Block those signals, and acid drops. That’s why H2 blockers like famotidine (Pepcid) and cimetidine (Tagamet) are used for heartburn, GERD, and ulcers.
They started showing up in the late 1970s after researchers realized histamine played a role in acid production. Before that, treatments were crude-antacids that gave short-term relief but didn’t stop the root cause. H2 blockers changed that. Famotidine can cut stomach acid by up to 75% for 12 hours. That’s longer than many antacids and faster than proton pump inhibitors (PPIs), which can take a day to build up their effect.
They’re not perfect. About 12% of users get headaches. Around 8% feel dizzy. Some have stomach upset-either constipation or diarrhea. And cimetidine has a big drawback: it interferes with how your liver processes other drugs. It can raise levels of blood thinners, antidepressants, and even some antibiotics. That’s why many doctors now prefer famotidine-it doesn’t mess with liver enzymes the same way.
Side Effects You Can’t Ignore
Side effects are where H1 and H2 blockers really split apart.
First-gen H1 blockers? Dry mouth, blurry vision, trouble peeing, and that heavy, hangover-like feeling the next day. About 25% of users report dry mouth. One in seven get blurry vision. For older adults, that’s a dangerous combo-increased fall risk, confusion, even delirium. One CareDash review from a caregiver said her 78-year-old mother became disoriented after taking Benadryl for allergies. It took three days to clear.
H2 blockers? Their side effects are milder but still real. Headache and dizziness are common. Gastrointestinal issues pop up in 10 to 15% of users. The bigger concern is long-term use. Some people find H2 blockers lose their punch after months-what’s called tachyphylaxis. That’s why some switch to PPIs. But PPIs come with their own risks: nutrient deficiencies, bone thinning, and increased infection risk. H2 blockers still have a place for people who can’t tolerate those.
There’s also a quiet risk with some H1 blockers: heart rhythm problems. The FDA issued warnings about high doses of certain antihistamines like astemizole and terfenadine (both pulled from the market) causing QT prolongation. Even today, if you take too much of any H1 blocker-especially with other meds that affect your heart-it can be dangerous.
When to Use Which One
Here’s the simple rule: H1 blockers for allergies. H2 blockers for stomach acid.
If you’re sneezing, itchy, or breaking out in hives, reach for an H1 blocker. Second-gen ones like loratadine or fexofenadine are best for daily use. If you’re getting heartburn after meals or waking up with acid in your throat, H2 blockers like famotidine are a solid choice. Take them 30 to 60 minutes before eating for best results.
Don’t use an H2 blocker for allergies. It won’t help. And don’t use an H1 blocker for heartburn-it won’t touch the acid. I’ve seen people take Benadryl for heartburn because they thought “antihistamine” meant “everything.” It doesn’t.
There’s one exception: severe allergic reactions. Even then, H1 blockers alone aren’t enough. For anaphylaxis, epinephrine is the only life-saving treatment. H1 blockers might help with itching or hives afterward, but they don’t stop airway swelling or blood pressure drop.
What’s New and What’s Changing
The H1 blocker market is growing. New drugs like bilastine (approved in 2021) barely enter the brain-less than 2% concentration compared to 15-20% in older ones. That means even less drowsiness, even for sensitive people.
On the H2 side, the big shift came in 2020 when ranitidine (Zantac) was pulled globally after traces of a cancer-causing chemical (NDMA) were found. That left famotidine as the main player. It’s still widely used, but it’s fighting a losing battle against PPIs, which dominate the acid-reduction market.
Still, H2 blockers have niche uses. The American Society of Anesthesiologists still recommends cimetidine for patients undergoing surgery to reduce stomach acid and prevent aspiration. It’s faster and safer than PPIs in that setting.
And here’s something surprising: researchers are now looking at combining H1 and H2 blockers for heart conditions. Early studies suggest blocking both receptors might help with heart failure by reducing harmful remodeling of heart tissue. Trials are underway, but this is still experimental.
What Real People Say
On Reddit’s r/Allergies, 68% of over 1,200 users said they stick to second-gen H1 blockers like Claritin because they don’t want to feel groggy. Only 22% use Benadryl-and most of them admit they take it at night to help sleep.
One user wrote: “I used to take Zyrtec for allergies. Then I started getting heartburn. I thought, ‘Maybe Zyrtec causes it?’ Turns out, it doesn’t. I just needed Pepcid. I was using the wrong tool for the job.”
For H2 blockers, reviews are mixed. Sixty-five percent say they work for heartburn. But 30% say the relief fades after a few weeks. One person said: “I took Pepcid every day for six months. Then one day, it stopped working. I had to switch to a PPI.”
On the flip side, someone with chronic hives tried five different H1 blockers before bilastine finally cleared it up. “After five years of itching, I slept through the night for the first time. No drowsiness. No trade-offs.”
Practical Tips
- If you’re using a first-gen H1 blocker like diphenhydramine, take it at bedtime. Avoid driving or operating machinery.
- For H2 blockers, take famotidine 30 to 60 minutes before meals if you know you’ll eat something spicy or acidic.
- Don’t mix H1 blockers with alcohol. It doubles the drowsiness risk.
- Check your other meds if you’re on cimetidine. It can interact with over 40% of common prescriptions.
- Don’t use H2 blockers long-term without checking in with your doctor. Tachyphylaxis is real.
- If you’re over 65, avoid first-gen H1 blockers entirely. Stick to loratadine, fexofenadine, or cetirizine.
Final Thoughts
H1 and H2 blockers are both antihistamines, but they’re not interchangeable. One treats your nose and skin. The other treats your stomach. Confusing them is like using a hammer to screw in a lightbulb-it won’t work, and you might hurt yourself.
Second-gen H1 blockers are safe, effective, and non-sedating for most people. H2 blockers like famotidine are reliable for acid relief and still hold value where PPIs aren’t suitable.
The key is matching the drug to the problem. Know what you’re treating. Know the side effects. And don’t assume all antihistamines are the same.
Can I take H1 and H2 blockers together?
Yes, but only under medical supervision. Some people with severe allergies or mast cell disorders take both. For example, someone with chronic hives might take loratadine (H1) and famotidine (H2) together if one alone isn’t enough. But combining them without a reason can increase side effects like dizziness or stomach upset. Don’t do it on your own.
Are H2 blockers safer than PPIs for long-term use?
For some people, yes. PPIs can lower magnesium, calcium, and vitamin B12 levels over time and increase the risk of bone fractures and gut infections. H2 blockers like famotidine don’t carry those same long-term risks. That’s why they’re still used for maintenance therapy in people who need ongoing acid control but can’t tolerate PPIs. They’re not as strong, but they’re often safer for years of use.
Why was Zantac taken off the market?
Ranitidine (Zantac) was pulled in 2020 because testing found it could break down into NDMA, a chemical linked to cancer. This happened even under normal storage conditions. The FDA ordered all products off shelves. Famotidine (Pepcid) and cimetidine (Tagamet) were never found to have this issue and remain available.
Do H1 blockers help with asthma?
Not directly. While histamine can trigger bronchoconstriction in some asthmatics, H1 blockers alone don’t reliably open airways. They might reduce mucus or itching in the throat, but they’re not a substitute for inhalers or bronchodilators. Some studies show H1 and H2 blockers together offer better bronchial protection than either alone, but this isn’t standard treatment. Always follow your asthma action plan.
Can I use H2 blockers for allergic reactions?
No. H2 blockers don’t block the histamine receptors involved in itching, swelling, or hives. That’s H1 receptors. If you’re having an allergic reaction, use an H1 blocker like cetirizine or diphenhydramine. For severe reactions, use epinephrine immediately. H2 blockers won’t help.
Which H1 blocker causes the least drowsiness?
Fexofenadine (Allegra) causes the least drowsiness among commonly used H1 blockers. Studies show it has near-zero sedation at standard doses. Loratadine (Claritin) is also very low-risk. Cetirizine (Zyrtec) causes mild drowsiness in about 10-15% of users, so it’s not ideal if you’re sensitive. Bilastine, newer and less common in the U.S., is even lower-less than 2% brain penetration.


Rod Wheatley
January 20, 2026 AT 18:16Okay, but can we talk about how everyone thinks Zyrtec is the holy grail? I switched to fexofenadine after my brain felt like it was wrapped in cotton for three days straight. No drowsiness. No brain fog. Just… freedom. 🙌
Ashok Sakra
January 22, 2026 AT 07:25Bro i took benadryl for heartburn and now my wife left me and my cat hates me 😭
Andrew Rinaldi
January 24, 2026 AT 07:12It's fascinating how two molecules with nearly identical names can have such divergent biological impacts. The body doesn't care about marketing labels-it responds to receptors. H1 for skin, H2 for stomach. Simple. Elegant. And yet, we still mix them up like it's a personality quiz. 🤔
Gerard Jordan
January 25, 2026 AT 13:12Just wanted to say-famotidine saved my life after that spicy taco incident. 🍔🔥 Also, if you’re over 65 and still taking Benadryl… please stop. Your brain will thank you. And your grandkids won’t have to explain why you’re hallucinating your cat is a robot. 🐱🤖
michelle Brownsea
January 27, 2026 AT 05:31Let me be crystal clear: Using first-generation H1 blockers after age 65 isn't just irresponsible-it's a public health failure. The American Geriatrics Society has issued a clear, evidence-based warning, and yet people still pop Benadryl like candy. This isn't 'natural remedy' territory-it's pharmacological negligence. Please, for the love of all that is neurologically intact, stop.
MAHENDRA MEGHWAL
January 27, 2026 AT 07:34Respectfully, I have observed that many individuals confuse the mechanism of action between H1 and H2 antagonists due to the shared terminology. The distinction is not merely academic; it is clinically significant. I have advised several patients to discontinue inappropriate use, and outcomes improved markedly. I encourage further education on receptor specificity.
Jarrod Flesch
January 28, 2026 AT 19:44Been using Allegra for years. Zero drowsiness. Zero drama. Just quiet, reliable allergy relief. Also, famotidine before curry? Chef's kiss. 🇦🇺
Glenda Marínez Granados
January 30, 2026 AT 06:35So you're telling me I didn't need to take Benadryl for my heartburn... I just needed to stop being a human who thinks 'antihistamine' = 'magic fix for everything'? 🙃
Yuri Hyuga
January 31, 2026 AT 19:26Excellent breakdown. I’ve seen patients self-prescribe H2 blockers for urticaria and wonder why it doesn’t work. This is precisely why medical literacy matters. Education isn’t optional-it’s preventative. Keep sharing this kind of clarity. 👏
Kevin Narvaes
February 2, 2026 AT 00:50wait so pepcid is for heartburn and zyrtec is for sneezing? i thought they were both just 'allergy pills' lol