What Are Hormone Therapy Combinations?
Hormone therapy combinations, often called HRT, are used to treat menopause symptoms like hot flashes, night sweats, and vaginal dryness. These treatments mix two hormones: estrogen and progestogen. The reason for combining them? If you still have a uterus, estrogen alone can cause the uterine lining to thicken - which raises the risk of endometrial cancer. Adding progestogen stops that growth. It’s not optional. It’s medical necessity.
For women who’ve had a hysterectomy, estrogen-only therapy is safe and common. But if you haven’t had your uterus removed, you need both. This isn’t a suggestion. It’s based on decades of research, including the Women’s Health Initiative, which showed clear risks when estrogen was used alone in women with intact uteri.
Two Main Types: Sequential vs. Continuous
There are two main ways to combine estrogen and progestogen: sequential and continuous. Which one you use depends on whether you’re still having periods or not.
Sequential HRT is for women in perimenopause or those who’ve had their last period within the last year. You take estrogen every day, then add progestogen for 10 to 14 days each month. This mimics your old cycle. You’ll likely get a withdrawal bleed - like a period - each month. It’s designed for women who still have some ovarian activity.
Continuous combined HRT is for women who haven’t had a period for 12 months or more. You take both hormones every single day, no breaks. No monthly bleeding. This is the standard for postmenopausal women. Studies show it lowers the risk of colon cancer by about 18% and type 2 diabetes by 21%, based on long-term WHI data.
Generic Options: What’s Actually in the Pills?
Most hormone therapy prescriptions today are generic. They’re cheaper, just as effective, and widely available. Here are the most common ones:
- Conjugated estrogens - 0.3mg, 0.45mg, or 0.625mg tablets. These are derived from horse urine and have been used for decades.
- Estradiol - 0.5mg or 1mg tablets. This is identical to the estrogen your body makes. Many doctors prefer it because it’s bioidentical.
- Medroxyprogesterone acetate - 2.5mg, 5mg, or 10mg tablets. A synthetic progestogen, widely used in combination pills.
Prices vary. In the U.S., you might pay $4 to $40 a month depending on your insurance and pharmacy. Generic estradiol with medroxyprogesterone can cost as little as $12 per month at Walmart or Costco with a GoodRx coupon.
But here’s the catch: not all generics are created equal. Some brands use different progestogens. Micronized progesterone (brand name Prometrium) is a natural form, derived from plants. It’s more expensive but has a better safety profile - especially for breast cancer risk.
Delivery Methods Matter More Than You Think
It’s not just about what you take - it’s how you take it. Oral pills are the most common, but they’re not the safest.
When you swallow hormones, they go straight to your liver. That stresses your liver and increases clotting factors. Oral estrogen raises your risk of blood clots by 2 to 3 times compared to patches or gels. The absolute risk is still low - about 1 in 1,000 women per year - but it adds up over time.
Transdermal options - patches, gels, sprays - bypass the liver. They’re absorbed through your skin. That means:
- Lower risk of blood clots
- Lower risk of stroke - especially important after age 60
- More stable hormone levels
For women with a history of high blood pressure, migraines with aura, or previous clots, transdermal is the only safe choice. In Europe, over 65% of HRT prescriptions are transdermal. In the U.S., it’s still only 35%. That’s changing, slowly.
There’s also the Mirena IUD - a small device placed in the uterus that releases progestogen directly. It’s great for women who want to avoid daily pills. You get endometrial protection without taking extra hormones by mouth. Many women use it with a low-dose estrogen patch.
Who Should Avoid HRT?
HRT isn’t for everyone. The biggest red flags:
- History of breast cancer
- History of blood clots, stroke, or heart attack
- Undiagnosed vaginal bleeding
- Active liver disease
- Known sensitivity to estrogen or progestogen
Age matters too. Starting HRT after 60, or more than 10 years after menopause, increases the risk of dementia, stroke, and heart disease. That’s why experts say: hormone therapy is for symptom relief, not disease prevention.
Dr. Gutierrez from Houston Methodist puts it bluntly: "Throwing hormones at a 70-year-old woman who hasn’t had them for 20 years is dangerous." The body changes. The risks change. What was safe at 50 isn’t safe at 65.
How Long Should You Stay on It?
There’s no fixed timeline. The goal is to use the lowest dose for the shortest time needed to control symptoms.
Most women take HRT for 2 to 5 years. Some need it longer - especially if symptoms are severe or they started early. The North American Menopause Society says to reassess every year after the first 3 to 5 years. Can you lower the dose? Switch to a patch? Try non-hormonal options like gabapentin for hot flashes?
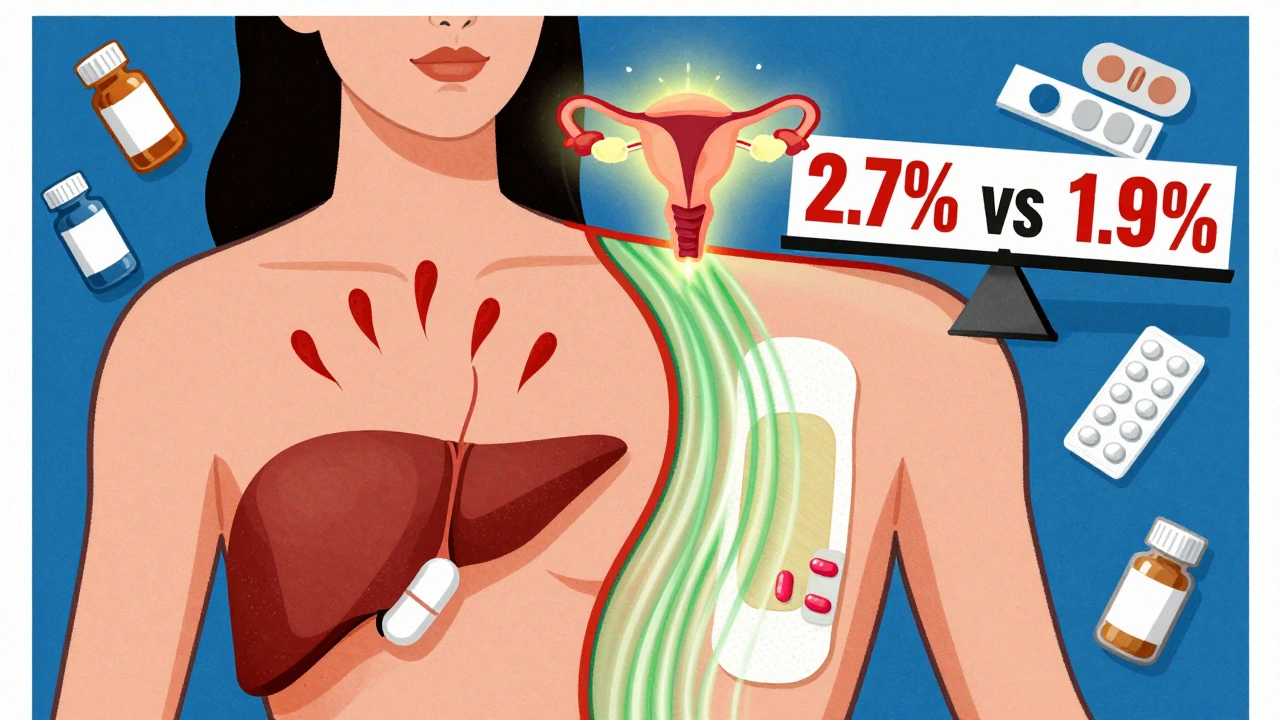
Long-term use (5+ years) of combined HRT slightly increases breast cancer risk. The data shows less than 1 in 1,000 women per year develop breast cancer because of HRT. But with synthetic progestins, that risk climbs by 2.7% per year. With micronized progesterone, it’s only 1.9%.
That’s why many doctors now prefer Prometrium over medroxyprogesterone - even if it costs more. The difference in breast cancer risk isn’t just statistical. It’s personal.
Side Effects and What to Do About Them
Breakthrough bleeding is the most common issue - especially in the first 6 months. Up to 20% of women on continuous HRT will spot or bleed. It’s usually harmless and fades with time. But if it lasts longer than 6 months, you need an ultrasound. It could be polyps, fibroids, or something more serious.
Other side effects: breast tenderness, bloating, mood swings, headaches. These often go away after a few weeks. If they don’t, your dose might be too high. Or your formulation isn’t right.
Try switching from oral to transdermal. Try micronized progesterone instead of medroxyprogesterone. Try a lower estrogen dose. Small changes make big differences.
And don’t ignore the mental side. Some women feel better emotionally on HRT. Others feel more anxious. It’s not all in your head. Hormones affect brain chemistry. If mood changes hit hard, talk to your doctor. There are alternatives.

What’s New in 2025?
Science hasn’t stood still. In 2023, the FDA approved a new transdermal patch that combines estradiol and micronized progesterone in one patch - the first of its kind. Early results from the TWIRP study suggest this combo may lower breast cancer risk even further than older pills.
Researchers are also testing tissue-selective estrogen complexes (TSECs) and selective progesterone receptor modulators (SPRMs). These are designed to give you the benefits of estrogen - for bones, brain, and hot flashes - without stimulating breast or uterine tissue. Several are in Phase III trials. They might be available by 2027.
For now, the best approach remains simple: use the lowest effective dose, choose transdermal if possible, prefer micronized progesterone over synthetics, and reevaluate every year.
Real-World Numbers You Should Know
Let’s put this in perspective:
- 1.4 million women in the U.S. are on systemic HRT (CDC, 2022)
- 78% of prescriptions are for generic formulations
- 12-15% of women aged 45-55 use HRT - only 4-6% of women over 65
- The global HRT market is growing at 3.8% a year - expected to hit $2.95 billion by 2030
Despite the stigma from the 2002 WHI study, HRT is making a comeback - but smarter this time. It’s no longer about "hormones for life." It’s about precision. Timing. Personalization.
Final Advice: Start Low, Go Slow, Reassess Often
If you’re considering HRT:
- Confirm you still have a uterus - if yes, you need progestogen.
- Choose transdermal estrogen over pills if you have any clotting, heart, or stroke risk.
- Ask for micronized progesterone (Prometrium) instead of medroxyprogesterone.
- Start with the lowest dose - 0.5mg estradiol, 100mg micronized progesterone.
- Give it 3 to 6 months to settle. Don’t quit too soon.
- Get a yearly check-up. Blood pressure, breast exam, pelvic ultrasound if bleeding persists.
- Don’t use HRT to prevent heart disease or dementia. It doesn’t work for that.
Hormone therapy isn’t a cure-all. But for women with moderate to severe menopause symptoms, it’s still the most effective treatment we have. Done right, it improves quality of life. Done wrong, it can cause harm. The difference? Knowing your options - and choosing wisely.

Ibrahim Yakubu
December 5, 2025 AT 22:32Brooke Evers
December 6, 2025 AT 11:03Chris Park
December 6, 2025 AT 22:05Saketh Sai Rachapudi
December 8, 2025 AT 04:02joanne humphreys
December 9, 2025 AT 00:50Kumar Shubhranshu
December 9, 2025 AT 19:53Mayur Panchamia
December 11, 2025 AT 05:09Karen Mitchell
December 12, 2025 AT 06:55Rashmi Gupta
December 13, 2025 AT 07:56