When you pick up a prescription, you might see two different dates on the bottle: one printed by the manufacturer, and another written by the pharmacy. One says expiration date. The other says beyond-use date. They look similar, but they’re not the same. Confusing them could mean taking a pill that doesn’t work-or worse, risking your health.
What Is an Expiration Date?
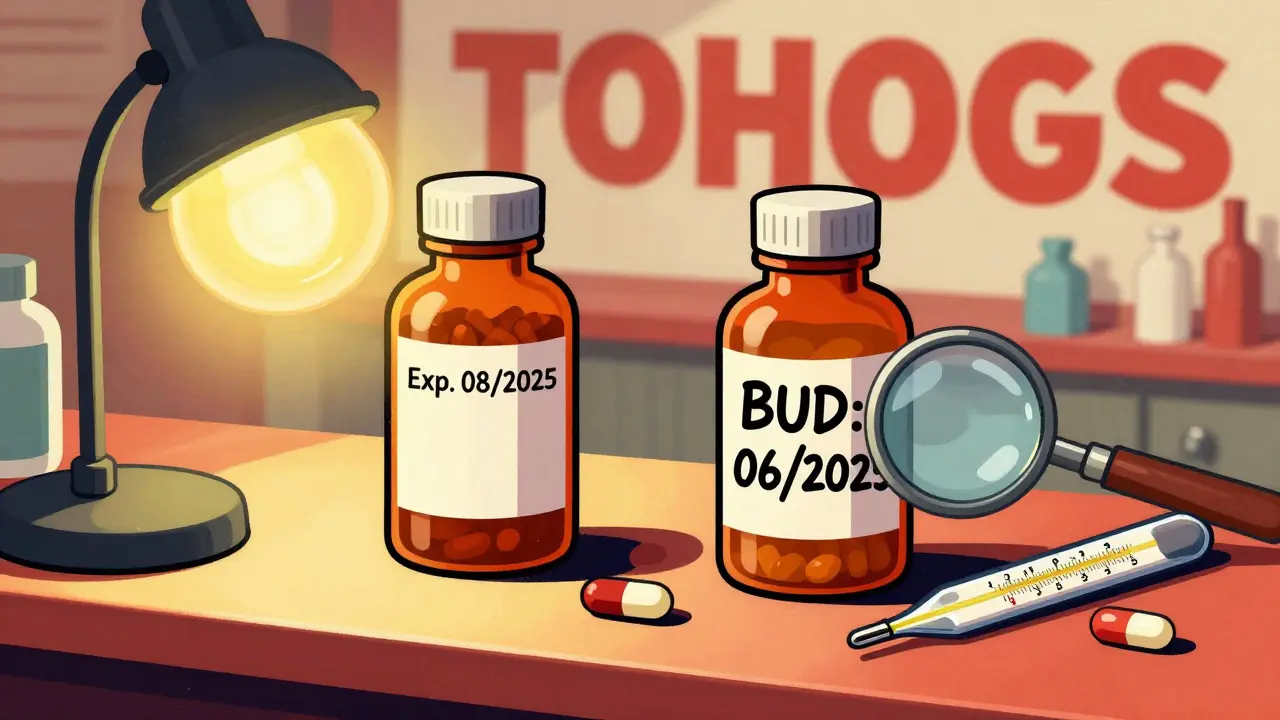
An expiration date comes from the drug manufacturer. It’s the last day they guarantee the medication is fully potent and safe to use, assuming it’s been stored correctly. This date isn’t random. It’s based on real science. Manufacturers test the drug under controlled conditions-heat, humidity, light-for months or years to see how it breaks down over time. The FDA requires this testing for every approved drug sold in the U.S. since 1979.For example, if your antibiotic bottle says "Exp. 08/2025," that means the manufacturer tested it and confirmed it still delivers at least 90% of its labeled strength up to that date. After that, they can’t promise it works as intended. The expiration date applies whether the bottle is open or sealed. If you keep it in a hot bathroom or a sunny windowsill, it might degrade faster. But the date itself doesn’t change.
Some people think expired drugs are dangerous. The FDA says that’s not usually true. In fact, a 2020 study found that 90% of over 100 tested drugs still worked fine 15 years past their expiration date-if stored perfectly. But here’s the catch: your home isn’t a lab. Temperature swings, moisture, and sunlight can ruin a drug long before its expiration date. That’s why the FDA still says: don’t use anything past its expiration date.
What Is a Beyond-Use Date?
A beyond-use date (BUD) is what you get when a pharmacy changes the medication. That could mean mixing powder into liquid for a child who can’t swallow pills. Or repackaging a tablet into a blister pack for an elderly patient. Or adding flavoring to make it taste better. Any time a pharmacist alters the original product, the manufacturer’s expiration date no longer applies.Instead, the pharmacist assigns a BUD. This date is based on guidelines from the United States Pharmacopeia (USP), not manufacturer testing. It’s a conservative estimate-how long the altered medication will stay safe and effective under typical storage conditions. Because compounded drugs lack the preservatives and stable packaging of commercial products, they’re more fragile.
For example, a compounded liquid suspension might have a BUD of just 14 days if kept refrigerated. A solid tablet that’s been repackaged might have a BUD of 6 months or up to a year, whichever comes first before the original expiration date. The BUD is always printed on the pharmacy label, usually in bold. If you don’t see it, ask your pharmacist.
Key Differences Between the Two Dates
Here’s how they stack up:
| Feature | Expiration Date | Beyond-Use Date (BUD) |
|---|---|---|
| Who sets it? | Manufacturer | Pharmacist |
| Based on? | FDA-approved stability testing | USP guidelines, pharmacist judgment |
| Applies to? | Unopened, unaltered commercial drugs | Compounded, repackaged, or altered drugs |
| Typical length | 1-5 years | 14 days to 1 year |
| Storage rules | Follow label instructions | Often stricter-e.g., refrigeration required |
| Legal authority | Federal (FDA) | State pharmacy boards, guided by USP |
One big mistake patients make: assuming the BUD on a compounded drug is the same as the manufacturer’s expiration date. A common scenario: You get a compounded thyroid medication. The original bottle says "Exp. 12/2026." The pharmacy label says "BUD: 06/2025." You think, "It’s still good for another year." But that’s wrong. The BUD overrides the expiration date because the drug was changed. After June 2025, it’s no longer safe-even if the original bottle says otherwise.
Why BUDs Are Shorter-and Why That Matters
Compounded medications don’t have the same protections as factory-made drugs. No preservatives. No sealed, moisture-proof packaging. No controlled manufacturing environment. Even something as simple as mixing a tablet with syrup can introduce bacteria or cause the active ingredient to break down faster.
USP guidelines classify compounded drugs by risk level:
- Low-risk: Simple mixing of commercial ingredients. BUD up to 34 days at room temperature.
- Medium-risk: Multiple ingredients, more complex prep. BUD up to 14 days refrigerated.
- High-risk: Sterile preparations (like IV bags). BUD often just 24-72 hours.
That’s why you might get a compounded liquid that needs to be kept in the fridge-even if the original pill didn’t. The pharmacist added water, which invites mold. They didn’t add preservatives, because the patient is allergic. So the clock starts ticking the moment it’s mixed.
A 2022 survey by the International Academy of Compounding Pharmacists found that 68% of patients threw away compounded meds before finishing their course-because the BUD ran out. That’s not just expensive. It’s dangerous. If you stop a course early because the drug expired, you risk the infection coming back stronger.
What Should You Do When You Get a New Prescription?
Here’s your simple checklist:
- Look at both labels. The manufacturer’s expiration date is on the original bottle or box. The BUD is on the pharmacy’s dispensed container.
- If the pharmacy repackaged your meds, the BUD is the one that matters-not the original expiration date.
- Check storage instructions. Compounded drugs often need refrigeration. Don’t assume it’s the same as the original.
- Write the BUD on your calendar. Set a reminder for 2-3 days before it expires so you can call the pharmacy to refill.
- Never use a drug past either date. Even if it looks fine.
And if you’re unsure? Ask your pharmacist. Say: "Is this a compounded medication? What’s the beyond-use date? Does it need to be refrigerated?" There’s no shame in asking. Pharmacists are trained to explain this.

What Happens If You Use an Expired or Overdue Drug?
Most of the time, you won’t get sick right away. But you might not get better, either. A weakened antibiotic won’t kill the infection. A degraded painkiller won’t take the edge off. In rare cases, chemical breakdown can create harmful byproducts.
For example, tetracycline antibiotics can degrade into compounds that damage the kidneys. Insulin loses potency over time, leading to uncontrolled blood sugar. Epinephrine auto-injectors (like EpiPens) can fail to deliver a full dose after expiration-potentially fatal in an allergic emergency.
The FDA and USP agree: if the date has passed, don’t take it. Not even one pill. The risk isn’t worth it.
What About Recycling Expired Medications?
Never flush them down the toilet or toss them in the trash. That pollutes water and risks accidental ingestion by kids or pets. Most U.S. pharmacies offer free take-back programs. In Scotland, pharmacies follow the same rules under the NHS. Drop off expired or unused meds at any pharmacy that displays the take-back logo.
Some communities have drug disposal bins at police stations or health clinics. Check with your local council. In Edinburgh, you can drop off expired meds at any NHS pharmacy-no questions asked.
Final Thought: Trust the Date, Not Your Gut
People say, "It still looks fine." Or, "I’ve taken this for years past the date." But drugs don’t spoil like milk. You can’t smell or see degradation. A pill might look perfect but have lost 40% of its strength. That’s not a guess-it’s science.
Expiration dates and beyond-use dates exist to protect you. One is a manufacturer’s promise. The other is a pharmacist’s safety net. Both are binding. Neither should be ignored.
If you rely on compounded meds-because you’re allergic to dyes, need a special dose, or have trouble swallowing pills-know your BUD like your birthday. Mark it. Set alerts. Call ahead. Don’t let a missed date cost you your health-or your money.

Erika Putri Aldana
December 21, 2025 AT 11:13Cameron Hoover
December 21, 2025 AT 17:16Stacey Smith
December 22, 2025 AT 08:52Ben Warren
December 23, 2025 AT 13:52Teya Derksen Friesen
December 25, 2025 AT 01:11Sandy Crux
December 25, 2025 AT 03:59Jason Silva
December 25, 2025 AT 05:13mukesh matav
December 26, 2025 AT 07:16Peggy Adams
December 26, 2025 AT 17:47Sarah Williams
December 27, 2025 AT 08:45Theo Newbold
December 29, 2025 AT 07:50