When you pick up your prescription, you might see a different name on the bottle than what your doctor wrote. That’s not a mistake. It’s probably a generic version of your medicine. And unless you’ve talked about it with your doctor, you might not even know the difference.
What’s the real difference between generic and brand-name drugs?
There’s a big myth out there: that brand-name drugs work better. They don’t. By law, a generic drug must contain the same active ingredient, in the same strength, and work the same way in your body as the brand-name version. The U.S. Food and Drug Administration (FDA) requires this. It’s not a suggestion-it’s a rule. If a generic doesn’t match the brand in absorption, safety, and effectiveness, it doesn’t get approved.
The only real differences? Price and appearance. Generics cost 80-85% less. A pill that might be $150 as a brand-name could be $20 as a generic. That’s not a small savings-it’s life-changing for people on fixed incomes or without good insurance.
Generics look different because of trademark laws. The shape, color, and even the imprint on the pill can’t match the brand. That’s why you might get a white oval one day and a blue capsule the next. It’s the same medicine. Just packaged differently.
Why do some people feel like generics don’t work as well?
It’s not usually the drug. It’s the mind.
When you’ve been taking a blue pill for years and suddenly get a white one, your brain can start whispering: Is this the same? Will it still work? That’s called the nocebo effect-the opposite of placebo. You expect it to be worse, so you feel worse.
Studies back this up. One survey by Kaiser Permanente found that 17% of patients worried when switched to a generic. But after a pharmacist explained the change, 92% were satisfied. Another study from Consumer Reports showed 89% of people noticed no difference in how the medicine worked.
There are rare exceptions. For drugs with a narrow therapeutic index-like warfarin, lithium, or some seizure meds-the window between a helpful dose and a dangerous one is tiny. Even small changes in how the body absorbs the drug can matter. That’s why some doctors still prescribe brand-name versions for these. But even here, the FDA says approved generics are safe. If your doctor insists on the brand, ask why. Is it because of your specific case? Or just habit?
How much money are you really saving?
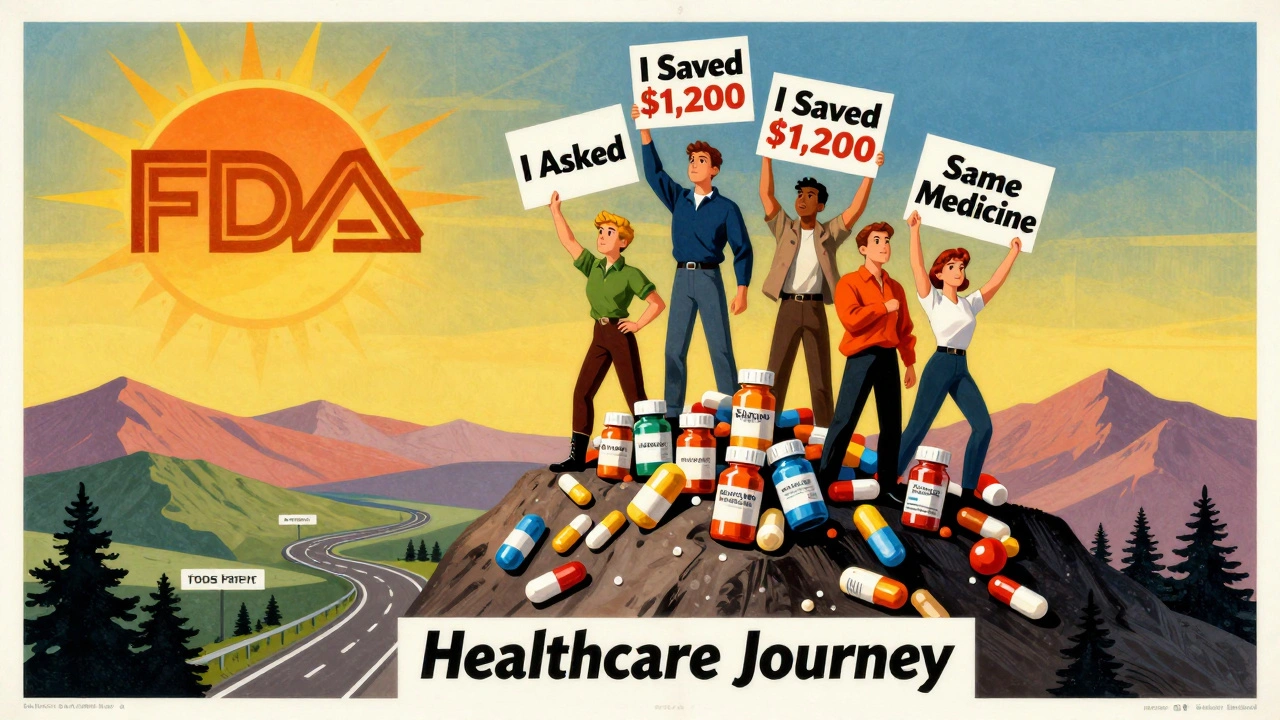
Let’s say you take a medication that costs $120 a month as a brand. The generic? $22. That’s $98 saved every month. Over a year? Nearly $1,200. That’s enough to cover a dental visit, a new pair of walking shoes, or a month’s worth of bus passes.
Across the whole U.S. healthcare system, generics saved $1.67 trillion between 2007 and 2016. In 2023, they saved patients an average of $45 per prescription. Nine out of ten prescriptions filled in the U.S. are for generics. But here’s the twist: brand-name drugs still make up 75% of total prescription spending. Why? Because they’re priced like luxury goods-even when they’re not.
If your doctor prescribes a brand-name drug, ask: Is there a generic? If they say no, ask: Why not? Sometimes it’s because they forgot. Sometimes it’s because they think you’ll do better on the brand. Sometimes it’s because they don’t know the cost difference. You’re not being pushy. You’re being smart.

What should you say to your doctor?
You don’t need to be an expert. Just be honest. Here are three simple questions to ask at your next visit:
- Is there a generic version of this medication? This opens the door. Most doctors know the answer.
- Will the generic work just as well for my condition? This shows you care about effectiveness, not just cost.
- Are there any reasons I should take the brand-name instead? This invites them to explain if there’s a real medical reason-not just tradition.
If you’ve had bad reactions to a generic before-even if it was just a rash or nausea-tell your doctor. That’s valuable info. Sometimes, it’s the inactive ingredients (like dyes or fillers) that cause issues, not the active drug. Your doctor can check if a different generic version might work better.
Also, mention if cost is a problem. Say it plainly: I’m struggling to afford this. Is there a cheaper option? Doctors hear this more than you think. They’ve seen people skip doses, split pills, or stop taking meds because of price. They want to help.
What if the pharmacy switches my drug without telling me?
In most U.S. states, pharmacies are required by law to substitute a generic if one is available-unless your doctor wrote “dispense as written” on the prescription. That’s legal. But it’s not always communicated well.
Always check your pill before you leave the pharmacy. Compare the shape, color, and name on the bottle to your last prescription. If it’s different, ask the pharmacist: Is this a generic? Is it the same as before? Pharmacists are trained to explain this. A 2022 study found that 78% of patient concerns about generics were resolved with a simple conversation.
If you’re confused or worried, don’t take it without asking. Call your doctor’s office. Ask if the switch was intentional. If you’re on a critical medication, like thyroid or heart medicine, don’t assume. Confirm.
Are there times when you should stick with the brand?
Yes-but they’re rare.
Biologic drugs, like those for rheumatoid arthritis or cancer, don’t have true generics. They have biosimilars. These are similar but not identical. They’re more complex to make, and sometimes, switching between them and the brand can cause issues. If you’re on one of these, talk to your specialist before any change.
Also, if you’ve been stable on a brand-name drug for years and it’s working perfectly, there’s no rush to switch. But don’t assume the generic won’t work just because you’ve never tried it.
And here’s one more thing: if you’re taking multiple medications, and one gets switched to a generic, your body might react differently to the combination. That’s why it’s important to report any new side effects-even if they seem small.
What’s changing right now?
The FDA approved 745 generic drugs in 2022-a 12% jump from the year before. More patents are expiring. More generics are coming. The average approval time for a generic dropped from 36 months to just 10 months thanks to better funding and processes.
But there’s a risk. About 45% of generic shortages are caused by manufacturing problems at single factories. If one plant in India or China has an issue, it can affect millions of people. That’s why some doctors still prefer brands for critical meds-because supply chains are fragile.
Still, the trend is clear: generics are the future. They’re safe, effective, and affordable. The only thing holding them back is fear-and misinformation.
Bottom line: You have the right to ask
Your doctor isn’t a gatekeeper. They’re a partner. And you’re the one living with the medication-its cost, its side effects, its impact on your life. You have every right to ask if a cheaper, equally effective option exists.
Don’t feel bad for asking. Don’t feel guilty for wanting to save money. Most doctors wish patients asked more often. They know the numbers. They know generics work. They just assume you don’t care-or that you already know.
Next time you’re handed a prescription, ask: Is there a generic? It’s simple. It’s powerful. And it might just change how you manage your health-for the better.


Emmanuel Peter
December 4, 2025 AT 19:58Look, I don't care what the FDA says - I took the generic for my blood pressure and felt like I was drowning in a vat of lukewarm Jell-O for three days. My heart was doing the cha-cha. The brand? Smooth as silk. Don't tell me it's all in my head when my body's screaming otherwise.
Ashley Elliott
December 5, 2025 AT 06:15My grandma switched to generic lisinopril last year after her Medicare deductible hit - and she’s been fine. No dizziness, no weird rashes, just cheaper pills and more money for her weekly bodega coffee. I think a lot of the fear comes from not knowing what’s in the pill - not because it’s less effective. Talk to your pharmacist. They’re the real heroes here.
Chad Handy
December 5, 2025 AT 22:31Okay, but let’s be real - the FDA’s approval process for generics is a joke. They test a handful of batches from one factory in Chennai, and then boom - millions of people get the same batch across 30 states. What if that factory’s got mold in the ventilation? What if the fillers are laced with cheap talc? We don’t know. They don’t test long-term. They don’t test interactions. They just check if it dissolves in water and call it a day. And now you’re telling me I should risk my life because it’s 80% cheaper? That’s not logic - that’s capitalism playing Russian roulette with your kidneys.
Augusta Barlow
December 6, 2025 AT 05:15Generics are a government conspiracy to make us dependent on cheap pills so we don’t notice how the pharmaceutical giants are still making billions off the inactive ingredients they sell to generic manufacturers. You think they don’t own the factories? They do. And the color changes? That’s to confuse you so you don’t realize you’re being dosed with a different chemical blend every month. I switched back to brand and my migraines stopped. Coincidence? I think not.
Joe Lam
December 6, 2025 AT 13:09Wow. Someone actually wrote a comprehensive, well-researched piece on generics. Imagine that. I’m shocked. Most people think ‘generic’ means ‘discount bin medicine’ - but no, it’s literally the same molecule. You’re not saving money by taking the brand. You’re just subsidizing Wall Street’s quarterly earnings. If you’re still paranoid after reading this, maybe your issue isn’t the pill - it’s your trust in science.
Carolyn Ford
December 8, 2025 AT 07:50...I’ve been on the same brand-name thyroid med for 12 years... and I’ve never had a single side effect... so why would I risk it?... I mean, sure, the FDA says it’s fine... but what about the *other* studies... the ones they don’t publish... the ones from Europe... where they track long-term outcomes...?... And what about the 2019 paper in The Lancet that showed...?... I mean, really...?... Are you just going to trust a government agency that also approved Vioxx?... I think not...
Yasmine Hajar
December 8, 2025 AT 20:54My cousin in Mexico got her diabetes meds from a pharmacy that didn’t even have a license - and she’s fine. But here? We’re scared of a white pill because it doesn’t look like the blue one we’ve had since 2014. It’s not about the medicine - it’s about control. We’re taught to fear change. But your body doesn’t care what color the pill is. It cares if it works. Ask for the generic. Try it. If it’s not right, go back. But don’t let fear cost you your health - or your rent.
Jake Deeds
December 9, 2025 AT 09:26It’s funny how people act like generics are some revolutionary breakthrough - as if we didn’t know this since the 1980s. I mean, come on. The real scandal is that we still pay brand prices for drugs that have been off-patent for decades. But no - we’re all just too lazy to ask. Too afraid to challenge the system. So we let Big Pharma turn our prescriptions into luxury items. And then we wonder why healthcare is broken. Spoiler: it’s because we let them.
Isabelle Bujold
December 9, 2025 AT 09:41As a pharmacist in Vancouver, I see this every day. Patients panic when their pill changes color - they think it’s a different drug. I show them the FDA equivalence sheet, the active ingredient list, the batch number. Nine times out of ten, they’re relieved. One time, a woman cried because she thought her doctor had switched her to a ‘lesser’ version. I asked her if she’d rather be alive and paying $20 a month - or dead and paying $150. She got it. Generics aren’t a compromise. They’re the standard. The brand is the exception - and it should be.
Jenny Rogers
December 11, 2025 AT 07:43It is not merely a matter of pharmacological equivalence, nor is it simply an economic consideration - it is, in fact, a profound moral imperative to interrogate the commodification of human health. To accept generics without critical inquiry is to capitulate to the neoliberal hegemony that reduces life-sustaining interventions to mere transactional commodities. The body is not a machine to be optimized for cost-efficiency; it is a sacred vessel - and to treat it otherwise is to commit a quiet, systemic sacrilege.
Scott van Haastrecht
December 13, 2025 AT 04:04Yeah, sure, the FDA says they’re the same. But have you seen the manufacturing plants? One in India had a rat in the mixing tank last year. And that’s just the one that got caught. I’ve got a friend who got a generic version of his antidepressant and ended up in the ER because his serotonin levels spiked. He didn’t know the pill was made by a company that got fined $200 million for falsifying data. You think that’s coincidence? Nah. It’s systemic. And you’re just too naive to see it.
Chase Brittingham
December 13, 2025 AT 18:55My dad’s on warfarin. Doctor kept him on brand because he’s got a narrow therapeutic window. But we called the pharmacy, found out there was a generic approved for it - same FDA rating. We asked the cardiologist again - he said, ‘Oh, yeah, I forgot that one’s approved now.’ He wasn’t being shady. He was just busy. So ask. Always ask. It’s not pushy - it’s your right. And if you’re scared, bring a friend to the appointment. I did. Best decision I ever made.