Why insomnia gets worse with age
More than one in three adults over 65 struggle with insomnia. It’s not just trouble falling asleep-it’s waking up at 3 a.m. and not being able to go back down, or waking up too early and feeling exhausted all day. These aren’t normal parts of aging. They’re medical problems that need the right solution.
As we get older, our bodies change. The brain produces less melatonin. Sleep cycles get shorter and lighter. Many seniors take multiple medications that interfere with sleep. And chronic conditions like arthritis, heart disease, or prostate issues mean nighttime pain or bathroom trips are common. All of this makes sleep harder to come by-and harder to keep.
The old solutions are dangerous
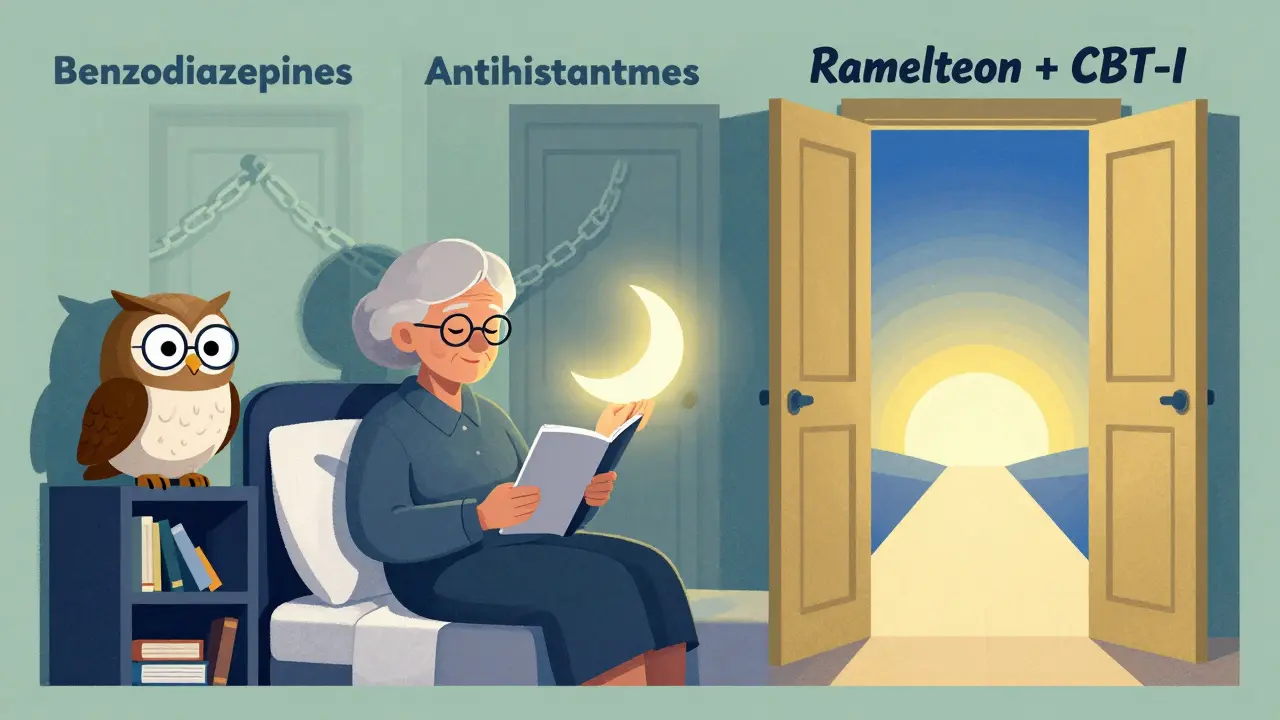
For decades, doctors reached for benzodiazepines like lorazepam or z-drugs like zolpidem (Ambien) to treat insomnia in older adults. These drugs worked-at first. But the risks started adding up.
Studies show that older adults on these medications are 50% more likely to fall and fracture a hip. One in five experiences next-day drowsiness that makes driving or walking unsafe. Some even sleepwalk, cook in their sleep, or drive while not fully awake. These aren’t rare side effects. They’re predictable outcomes.
The American Geriatrics Society banned these drugs as first-line treatments back in 2012. Yet in 2023, nearly 7.2 million Medicare beneficiaries still got benzodiazepines for sleep. That’s not because they’re effective. It’s because better options weren’t offered.
The safest options, backed by science
When medication is needed, the goal isn’t to knock you out. It’s to gently help your body return to natural sleep patterns-with the least risk.
Low-dose doxepin (3-6 mg) is FDA-approved specifically for sleep maintenance in older adults. At this tiny dose, it doesn’t act as an antidepressant. It blocks histamine receptors, which helps you stay asleep without grogginess the next day. In clinical trials, it improved total sleep time by over 40 minutes and had the lowest rate of next-day drowsiness among all sleep meds studied. Generic versions cost under $15 a month.
Ramelteon (8 mg) mimics melatonin and helps reset your internal clock. It’s ideal if you struggle to fall asleep but don’t wake up often. It doesn’t cause dependence, memory issues, or falls. Studies show it reduces sleep onset time by about 10 minutes. It’s not a powerhouse, but it’s one of the safest.
Lemborexant (5-10 mg) is newer but well-studied in seniors. It works by blocking orexin, a brain chemical that keeps you awake. Unlike older drugs, it doesn’t suppress breathing or cause deep sedation. In a 12-month trial with adults over 65, it added 42 minutes of sleep per night and reduced nighttime awakenings by over 20 minutes. Only 12% reported dizziness-and most of that faded within two weeks.
What to avoid
Even if a doctor says it’s "mild," avoid these:
- Benzodiazepines (lorazepam, temazepam, triazolam): High fall risk, memory loss, dependency
- Z-drugs (zolpidem, eszopiclone, zaleplon): Risk of sleepwalking, confusion, next-day impairment
- Antihistamines (diphenhydramine, doxylamine): Found in OTC sleep aids like Benadryl or Unisom. They cause dry mouth, constipation, urinary retention, and confusion in seniors.
- Sedating tricyclics (amitriptyline, nortriptyline): Used off-label for sleep, but increase heart rhythm risks and dizziness.
These drugs don’t just cause side effects-they can accelerate cognitive decline. A 2025 study found that seniors on these medications had a 27% higher risk of becoming disabled within a year, even after adjusting for other health issues.

Real stories from real seniors
On patient forums, the same pattern keeps appearing:
- "I was on Ambien for years. One morning, I woke up in the kitchen in my pajamas, making coffee. I didn’t remember walking there. My daughter made me stop."
- "Doxepin 3mg gave me 5 extra hours of sleep without the hangover. My doctor said it was for depression, but I didn’t feel depressed. He just didn’t know it worked for sleep too."
- "Lemborexant worked great, but $750 a month? I can’t afford it. I switched back to doxepin-and I’m fine."
Cost matters. Lemborexant and suvorexant are expensive. Most Medicare plans require prior authorization. But doxepin and ramelteon are affordable, accessible, and backed by decades of safety data.
What your doctor should check before prescribing
Safe prescribing isn’t just about picking the right drug. It’s about checking the whole picture.
A good doctor will:
- Ask you to keep a sleep diary for two weeks before prescribing anything
- Test your fall risk with a simple Timed Up and Go test (time how long it takes to stand from a chair, walk 10 feet, turn, walk back, and sit down)
- Check your liver and kidney function-many sleep meds are cleared by these organs
- Review every medication you take. CYP3A4 inhibitors (like certain antibiotics or antifungals) can double or triple the effect of z-drugs
- Ask if you’ve tried CBT-I (Cognitive Behavioral Therapy for Insomnia)
Only 32% of seniors prescribed sleep meds get a proper sleep assessment first. That’s not care. That’s prescription by default.
Non-drug options you should try first
CBT-I is the most effective treatment for insomnia in older adults-and it’s drug-free. It teaches you how to fix thoughts and habits that keep you awake. Studies show it works better than any medication, and the benefits last for years.
Here’s what it includes:
- Restricting time in bed to match actual sleep (sleep restriction)
- Getting out of bed if you can’t sleep after 20 minutes (stimulus control)
- Managing anxiety about sleep
- Improving sleep environment (light, noise, temperature)
Many community centers, VA hospitals, and telehealth services now offer CBT-I programs. Some are even covered by Medicare. Ask your doctor for a referral.
When to stop and when to keep going
Most sleep meds should be used short-term-no longer than 4 to 6 weeks. The goal isn’t lifelong dependence. It’s to break the cycle of poor sleep so your body can heal itself.
Low-dose doxepin is an exception. Because it doesn’t cause tolerance or dependence, it can be used long-term if needed. But even then, it should be reviewed every 6 months.
Set a date to reassess. Mark it on your calendar. Ask yourself: Am I sleeping better? Am I falling less? Do I feel more alert in the morning? If the answer is yes, you might not need the drug anymore.
What’s coming next
New drugs are on the horizon. Danavorexton, a selective orexin agonist, is in late-stage trials and could offer a new way to promote natural sleep without sedation. It’s not available yet, but it shows where the field is heading: away from brain-suppressing drugs and toward smarter, safer sleep regulation.
For now, the best tools are already here: low-dose doxepin, ramelteon, and CBT-I. They’re proven. They’re affordable. They’re safe.
Final thought: Sleep isn’t a weakness
Insomnia isn’t something you just have to live with. It’s not "just getting old." It’s a treatable condition that affects your safety, your health, and your quality of life. You deserve to sleep well-not just to be drugged into it.
Ask your doctor: "What’s the safest option for me?" And if they don’t mention CBT-I or low-dose doxepin, ask why.
Is it safe to take melatonin supplements for insomnia in older adults?
Controlled-release melatonin (2 mg) is considered safe and effective for sleep onset issues in older adults. Unlike OTC melatonin pills (which often contain 3-10 mg and aren’t regulated), the 2 mg controlled-release version mimics your body’s natural melatonin pattern. It’s been shown to reduce the time it takes to fall asleep by about 10 minutes with no next-day grogginess or fall risk. Avoid high-dose melatonin-it can cause dizziness and disrupt natural hormone cycles.
Can I stop my sleep medication cold turkey?
No. Stopping benzodiazepines or z-drugs suddenly can cause rebound insomnia, anxiety, or seizures. Always taper under medical supervision. Even with safer drugs like lemborexant, it’s best to reduce slowly. Work with your doctor to create a step-down plan over 2-4 weeks. Combine tapering with CBT-I to reduce withdrawal symptoms and prevent relapse.
Why isn’t my doctor prescribing doxepin for sleep?
Many doctors aren’t trained on low-dose doxepin for sleep. They know it as an antidepressant, but not that 3-6 mg is FDA-approved for insomnia and works differently at that dose. Bring up the 2010 FDA approval and ask if they’ve considered it. If they say it’s off-label, clarify: it’s FDA-approved for this exact use. You can also ask for a referral to a sleep specialist.
Are over-the-counter sleep aids safe for seniors?
No. Most OTC sleep aids contain diphenhydramine or doxylamine-antihistamines that cause confusion, dry mouth, urinary retention, and constipation in older adults. They also impair memory and increase fall risk. The American Academy of Sleep Medicine advises against them for seniors. Even "natural" labels don’t make them safe. Stick to evidence-based options like melatonin or prescription meds.
How long does it take for safer sleep meds to work?
Ramelteon and low-dose doxepin usually show results within 3-7 days. Lemborexant may take up to 2 weeks to reach full effect. Don’t expect instant results. The goal isn’t to fall asleep instantly-it’s to restore natural sleep patterns. Give it time. Track your sleep with a simple diary: bedtime, wake time, how many times you woke up, how you felt in the morning. That helps you and your doctor see progress.


Saylor Frye
January 4, 2026 AT 15:12Also, lemborexant at $750/month? That’s not a sleep aid, that’s a luxury subscription. Who even has Medicare Part D that covers this? The system is rigged.
Kiran Plaha
January 6, 2026 AT 02:00Isaac Jules
January 7, 2026 AT 08:52Amy Le
January 8, 2026 AT 05:21Pavan Vora
January 9, 2026 AT 00:31Indra Triawan
January 10, 2026 AT 08:42Harshit Kansal
January 11, 2026 AT 07:58Brian Anaz
January 12, 2026 AT 01:15