Isoniazid Hepatotoxicity Risk Calculator
Risk Factors
Enter your health details to assess your risk of isoniazid-induced liver damage.
When you take isoniazid for tuberculosis, you're not just fighting one infection-you're managing a complex chemical dance inside your liver. This drug, used for over 70 years, is still one of the most common treatments for TB worldwide. But behind its effectiveness lies a quiet danger: liver damage. And it's not random. It follows patterns tied to your genes, what other drugs you're taking, and even how much you drink.
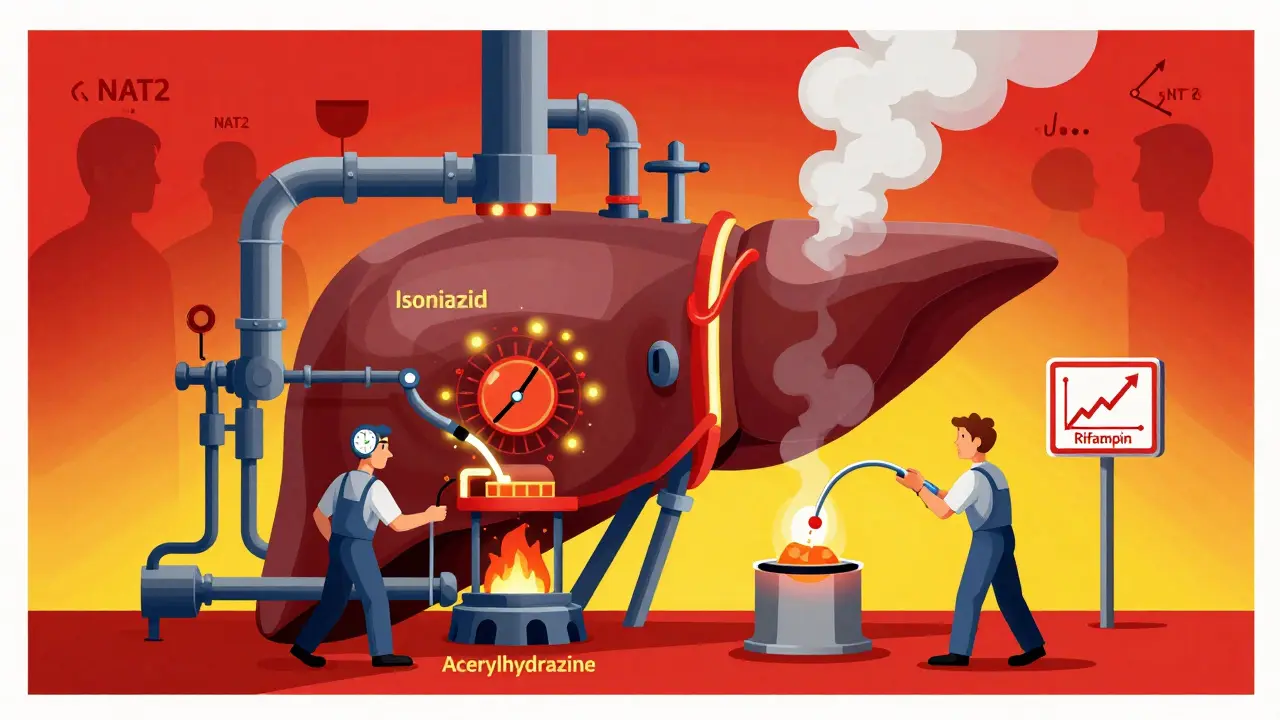
Why Isoniazid Hits the Liver Hard
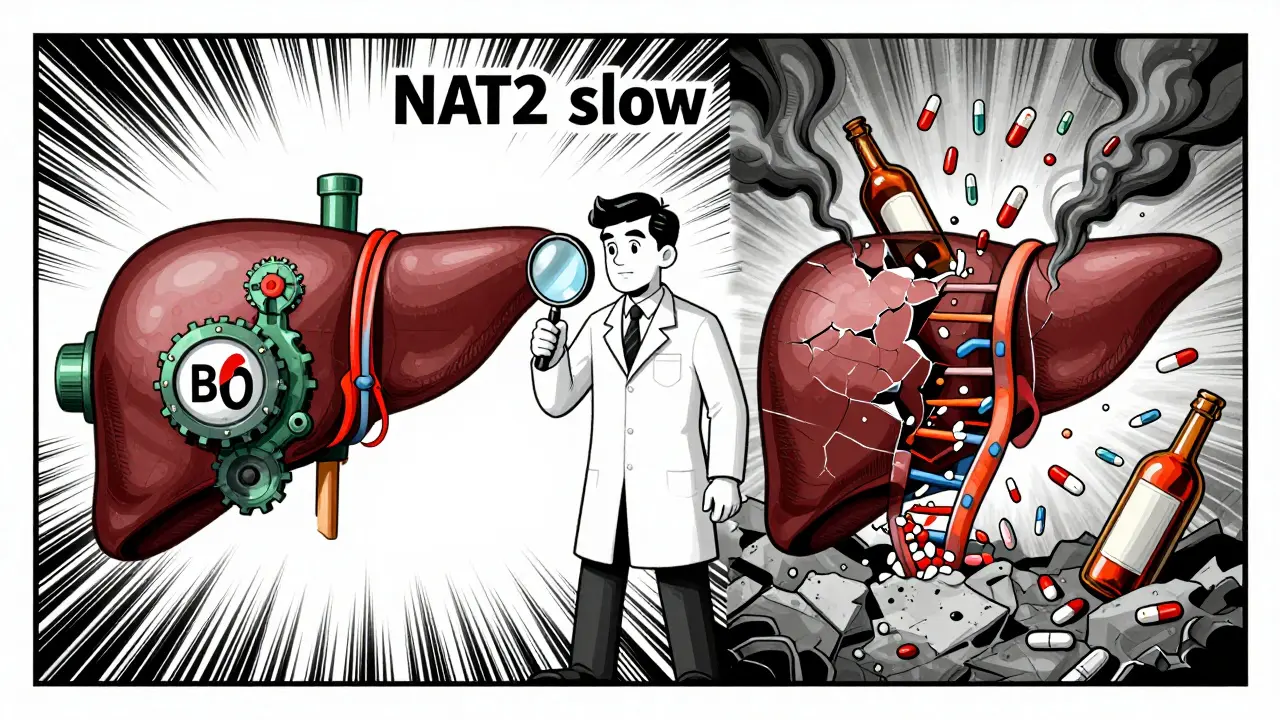
Isoniazid works by stopping the TB bacteria from building its protective outer layer. But your body doesn't handle it cleanly. About 75-95% of the drug gets broken down in your liver, and some of those breakdown products are toxic. These metabolites, especially acetylhydrazine, bind to liver cells, trigger inflammation, and disrupt energy production in mitochondria. That’s why liver enzymes like ALT and AST go up-your liver is under stress.Not everyone reacts the same way. Your risk depends heavily on whether you're a slow or fast acetylator. This isn't about how fast you digest food-it's about a gene called NAT2. About 40-70% of people in Europe and North America are slow acetylators. In South Africa, that number jumps to nearly 87%. Slow acetylators process isoniazid too slowly, so the drug and its toxic byproducts hang around longer, increasing liver damage risk by more than 2.5 times compared to fast acetylators.
A 2016 study of 85 TB patients found that 96% of those who developed liver injury were slow acetylators. Their average isoniazid exposure (measured as AUC) was nearly 45% higher than those who didn’t get sick. For them, even a standard 300 mg daily dose becomes a ticking time bomb.
The Perfect Storm: When Isoniazid Meets Other Drugs
Isoniazid rarely acts alone. Most TB patients get it with rifampin and pyrazinamide. That’s where things get dangerous.Rifampin, meant to help kill TB, actually makes isoniazid more toxic. It turns on liver enzymes-CYP2E1 and CYP3A4-that speed up the conversion of isoniazid into acetylhydrazine. Think of it like revving an engine while dumping gasoline into the fuel tank. Studies show that combining isoniazid with rifampin increases liver injury risk from 2-5% (with isoniazid alone) to 5-15%.
Pyrazinamide adds another layer. The standard 2-month HRZE regimen (isoniazid, rifampin, pyrazinamide, ethambutol) carries a 10-20% chance of liver damage. That’s nearly double the risk of a simpler 4-month HR regimen. The CDC and WHO both warn that this combo isn't just more effective-it's more dangerous.
And it doesn’t stop there. Isoniazid itself blocks liver enzymes like CYP2E1 and CYP2C. That means if you're also taking seizure meds like phenytoin or carbamazepine, those drugs build up in your blood. One study showed levels rising by 55-57%. That’s not just a lab curiosity-it can lead to seizures, dizziness, or even coma.
Who’s Most at Risk?
It’s not just about genetics. Certain conditions make liver damage from isoniazid much more likely:- Age: People over 35 have higher risk-liver function declines with age.
- Alcohol use: More than 14 drinks a week for men, or 7 for women, triples your risk. Alcohol and isoniazid both stress the same liver pathways.
- Pre-existing liver disease: If your ALT is already over 3 times the normal level, don’t start isoniazid without a specialist’s input.
- Malnutrition or diabetes: These weaken your liver’s ability to detoxify.
- Women, especially postpartum: Hormonal changes seem to increase susceptibility.
One study found that 70% of liver injury cases were mild and resolved even if patients kept taking the drug. But 30% became severe-requiring immediate stoppage. Symptoms like nausea, vomiting, abdominal pain, or dark urine shouldn’t be ignored. Jaundice (yellow skin) or clay-colored stools? That’s an emergency.
Monitoring and Prevention: What Doctors Should Do
There’s no magic test to predict who’ll get liver damage. But there are clear steps to reduce risk:- Baseline LFTs: Check liver enzymes before starting isoniazid. If they’re already high, reconsider the regimen.
- Monthly monitoring: For asymptomatic patients, check ALT every 4 weeks. For high-risk groups (slow acetylators, alcohol users), check every 2 weeks.
- Stop the drug if: ALT exceeds 5× ULN with symptoms, or 8× ULN without symptoms. This is the CDC’s hard line.
- Pyridoxine (vitamin B6): Give 25-50 mg daily to everyone on isoniazid. It prevents nerve damage, which affects up to 20% of users-and up to 50% in slow acetylators.
- Genetic testing? Not routine yet, but in Europe, the EMA recommends it for high-risk populations. In the U.S., it’s still rare. But if you’re of African or South Asian descent and have family history of liver problems, ask about NAT2 testing.
Newer Regimens Are Changing the Game
The future of TB treatment is moving away from isoniazid. In 2022, the WHO approved a new 4-month regimen using rifapentine and moxifloxacin. It cuts isoniazid exposure from 6-9 months down to just 4. Early data shows a 30-40% drop in liver injury risk.Even more promising is the BPaLM regimen (bedaquiline, pretomanid, linezolid, moxifloxacin), approved for drug-resistant TB in 2023. It completely removes isoniazid. For patients who can’t tolerate it-or who have resistant strains-this is a game-changer.
Still, isoniazid remains essential. In low-income countries, a single 300 mg tablet costs $0.03. New regimens cost over $100 per course. That’s why 95% of global TB treatment still includes isoniazid. But the trend is clear: less exposure = less liver damage.

What You Should Know If You’re Taking Isoniazid
If you’re on isoniazid for latent TB or active disease:- Don’t skip your liver tests. Even if you feel fine.
- Report any nausea, fatigue, or dark urine immediately.
- Avoid alcohol completely while on treatment.
- Take your vitamin B6 daily. It’s not optional-it’s protective.
- Tell your doctor about every other medication, supplement, or herb you take. Even over-the-counter painkillers like acetaminophen can add risk.
Recovery from isoniazid liver injury is usually complete. In the 2016 study, 95% of patients recovered fully within 4-8 weeks after stopping the drug. But you can’t afford to wait for symptoms. Prevention is the only safe strategy.
What’s Next?
Researchers are testing liver-protecting agents like silymarin (milk thistle extract). A 2021 study showed a 27% reduction in liver injury when it was added to isoniazid therapy. It’s not standard yet, but it’s a sign of where the field is headed: personalized, protective, and precise.For now, the answer isn’t to avoid isoniazid-it’s to use it smarter. Know your risk. Monitor closely. Don’t ignore the signs. And if you’re a slow acetylator, have a plan with your doctor before you even start.
Can isoniazid cause permanent liver damage?
Permanent liver damage from isoniazid is rare. In most cases, liver enzymes return to normal within 4-8 weeks after stopping the drug. Severe cases (like liver failure) are extremely uncommon-fewer than 1 in 10,000 patients. The key is early detection. If you stop isoniazid at the first sign of rising liver enzymes, recovery is nearly guaranteed.
Is it safe to take acetaminophen (Tylenol) with isoniazid?
It’s risky. Both isoniazid and acetaminophen are processed by the same liver enzymes. Taking them together increases the chance of liver injury, especially if you drink alcohol, are overweight, or are a slow acetylator. If you need pain relief, talk to your doctor. Alternatives like ibuprofen (if kidney function is normal) are often safer.
Do I need genetic testing for NAT2 before starting isoniazid?
Not routinely-but you should ask if you’re at high risk. If you’re over 35, have a history of liver disease, drink alcohol regularly, or are from a population with high slow-acetylator rates (like South Africa or parts of Asia), testing can help guide your treatment. In Europe, it’s recommended. In the U.S., it’s still not standard, but some clinics offer it for high-risk patients.
Can I restart isoniazid after liver injury?
Never restart isoniazid after a severe reaction. If you had symptoms like jaundice, nausea, or ALT over 5× ULN, the drug should be permanently avoided. Re-challenging-even months later-can cause rapid, life-threatening liver failure. Your doctor will switch you to an alternative regimen like rifapentine-moxifloxacin or BPaLM.
How long does it take for liver enzymes to return to normal after stopping isoniazid?
Most people see improvement within 2-4 weeks. Full recovery usually takes 4-8 weeks. Your doctor will monitor your ALT and AST levels until they return to normal. If enzymes haven’t improved after 8 weeks, further testing for other liver conditions is needed.
Is isoniazid still worth taking given the risks?
Yes-if managed properly. Isoniazid reduces the risk of active TB by up to 90% in latent infection. For millions of people, it’s the only affordable, effective option. The key is not avoiding it, but using it with caution: monitor your liver, avoid alcohol, take vitamin B6, and report symptoms early. The benefits far outweigh the risks when used correctly.