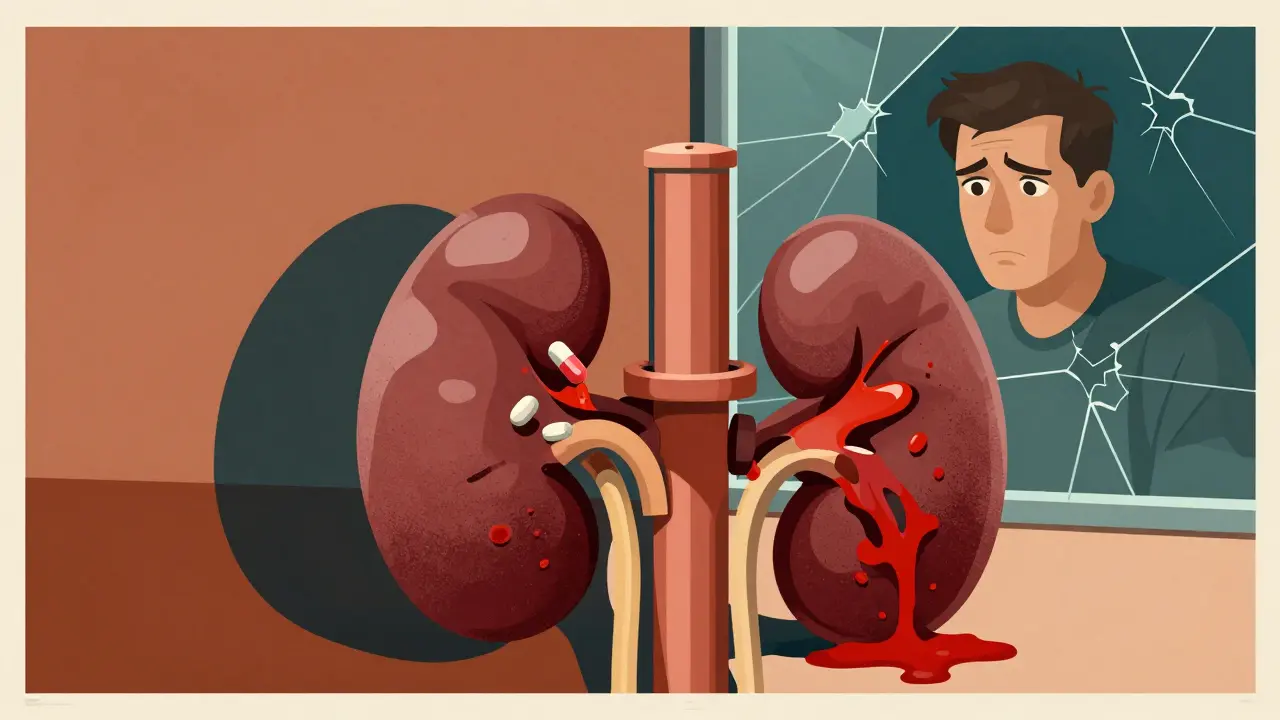
When your kidneys aren’t working right, your body can’t flush out medicines like it should. That means drugs you take for high blood pressure, diabetes, or even a simple headache can build up to dangerous levels. It’s not rare. In fact, medication accumulation is one of the most common-and preventable-causes of kidney damage in people with chronic kidney disease (CKD). And it’s happening to far too many people who don’t even realize their meds are hurting them.
Why Your Kidneys Matter for Medicines
Your kidneys don’t just make urine. They filter about 30% of all medications out of your blood every day. When kidney function drops, those drugs stick around longer. That’s not a minor issue. It turns safe doses into toxic ones. The National Kidney Foundation says 37 million Americans have CKD. Many of them are on 10 or more prescriptions a day-for heart disease, diabetes, arthritis, depression. Each one of those meds has to be handled differently when your kidneys are weak.What Happens When Drugs Build Up
Imagine taking ibuprofen for back pain. Normal dose? Fine. But if your eGFR (a measure of kidney function) is below 60, that same pill can cut off blood flow to your kidneys. Within days, your creatinine spikes. You end up in the hospital. That’s not a fluke. Studies show NSAIDs like ibuprofen, naproxen, and diclofenac triple the risk of acute kidney injury in people with CKD. And many don’t even know they have kidney disease until they get sick from a common painkiller. It’s not just pain meds. Take metformin, the most common diabetes drug. It’s safe for most people. But if your eGFR drops below 30, your body can’t clear lactic acid properly. That leads to lactic acidosis-a life-threatening condition. The good news? If you stop metformin when your eGFR hits 30, the risk drops to near zero. The problem? Many doctors still prescribe it at full dose.High-Risk Medications You Need to Watch
Some drugs are especially dangerous when your kidneys are failing. Here’s what to know:- NSAIDs: Avoid completely if your eGFR is below 30. Even at 60, use them only for a few days.
- Sulfonylureas: Chlorpropamide and glyburide can cause days-long low blood sugar. Glipizide is safer-no dose change needed.
- Trimethoprim: Often in antibiotics like Bactrim. When taken with blood pressure meds like ACE inhibitors, it can spike potassium to deadly levels. One study showed potassium rising 1.8 mmol/L in just 48 hours.
- Aciclovir: Used for shingles and cold sores. Can form crystals in your kidneys. Risk jumps if your eGFR is below 50.
- DOACs: Apixaban and rivaroxaban are blood thinners. They’re easier than warfarin-but they build up fast in CKD. Bleeding risk goes up 40% in stage 4 kidney disease.
- Calcineurin inhibitors: Tacrolimus and cyclosporine are life-saving after transplants. But their window between helpful and harmful is razor-thin. Toxicity can start within days.
These aren’t hypothetical risks. Patients on Reddit and patient forums report real stories: creatinine jumping from 1.8 to 3.2 after one week of ibuprofen. Severe hypoglycemia after taking glyburide for years at the same dose. Emergency trips because potassium hit 6.5. These are preventable disasters.

How Doctors Miss the Signs
Here’s the scary part: many providers don’t check kidney function before prescribing. A JAMA Internal Medicine study found that in 35% of primary care visits, doctors never calculated eGFR-they just looked at serum creatinine. That’s like judging a car’s fuel efficiency by how much gas is in the tank, without knowing if the engine’s broken. Even when eGFR is known, dosing errors are common. The American Society of Health-System Pharmacists found that 42% of prescriptions for drugs cleared by the kidneys were wrong in patients with CKD. Why? Outdated guidelines. Assumptions. Lack of training. And too many meds on the list.What You Can Do Right Now
You don’t have to wait for your doctor to catch it. Take control:- Know your eGFR. Ask for it at every visit. Don’t accept “your creatinine is normal” without seeing the number. If it’s below 60, your meds need review.
- Make a full med list. Include every pill, supplement, and OTC drug. Bring it to every appointment. Highlight anything you take for pain, blood sugar, or infection.
- Ask: “Is this safe for my kidneys?” Don’t be shy. Say: “My eGFR is 45. Does this dose need to change?”
- Use a tool. Apps like Meds & CKD (from Healthmap Solutions) let you scan your meds and get instant risk alerts. Users report 82% better conversations with their doctors after using it.
- Watch for warning signs. Dizziness, confusion, extreme fatigue, irregular heartbeat, or swelling could mean drug toxicity. Don’t wait. Call your provider.
New Tools Are Changing the Game
Technology is catching up. In 2023, the FDA approved KidneyIntelX-a machine learning tool that predicts your personal risk of drug toxicity based on your kidney function, age, other meds, and genetics. It’s 89% accurate. Hospitals are starting to use it. Electronic health records are also getting smarter. Stanford researchers predict that by 2030, your doctor’s computer will auto-flag unsafe prescriptions before they’re even written. That’s huge. Meanwhile, the KDIGO guidelines (updated in 2023) now require all new drugs to include clear kidney dosing instructions. The FDA is fining companies $2.5 million if they don’t. That’s forcing change.
It’s Not Just About Avoiding Bad Drugs
Some newer medications actually protect your kidneys. SGLT2 inhibitors like dapagliflozin and empagliflozin, originally for diabetes, are now used to slow CKD progression. But here’s the catch: they need dose adjustments when eGFR drops below 45. Miss that, and you lose the benefit-or risk side effects. The bottom line? Kidney disease doesn’t mean you can’t take meds. It means you need them smarter. Every pill you take has to be reviewed through the lens of your kidney function. What was safe last year might be dangerous this year.The Cost of Getting It Wrong
Drug-induced kidney injury adds $10,000 to $15,000 per hospital stay. Medicare spent $18.7 billion in 2022 on preventable hospitalizations linked to unadjusted meds in CKD patients. And 65% of those cases could have been avoided with simple checks. This isn’t just a medical issue. It’s a systemic failure. But it’s fixable.People with CKD are not helpless. You can ask questions. You can track your numbers. You can demand better. The data is clear. The tools exist. The guidelines are updated. What’s missing is awareness-and action.
Can I still take ibuprofen if I have kidney disease?
If your eGFR is below 60, avoid ibuprofen and other NSAIDs unless your doctor says it’s safe for a few days. If your eGFR is below 30, do not take them at all. They can cause sudden kidney injury, even if you feel fine. Use acetaminophen instead for pain, but check with your doctor first.
How do I know if my medication dose needs to change for kidney disease?
Ask your pharmacist or doctor to check your eGFR and compare it to the drug’s renal dosing guidelines. Any drug cleared by the kidneys (over 50%) usually needs adjustment when eGFR falls below 60. Common ones include metformin, antibiotics, blood thinners, and diabetes pills. Use tools like Meds & CKD or the FDA’s renal dosing database to verify.
Is metformin safe for people with kidney disease?
Yes-if dosed correctly. Stop metformin if your eGFR drops below 30. Reduce the dose if your eGFR is between 30 and 45. Studies of 20,000 patients show no cases of lactic acidosis when these rules are followed. Never take metformin if you’re dehydrated, having surgery, or getting contrast dye.
What’s the difference between eGFR and serum creatinine?
Serum creatinine is a single number from a blood test. It doesn’t tell you how well your kidneys are working by itself. eGFR is a calculated number that adjusts for your age, sex, race, and creatinine level. It gives a much better picture of kidney function. Always ask for your eGFR-not just creatinine.
Can herbal supplements harm my kidneys if I have CKD?
Yes. Many herbs like aristolochic acid, licorice root, and certain weight-loss supplements are directly toxic to kidneys. They’re not regulated like prescription drugs, so their kidney risks aren’t always known. Always tell your doctor about every supplement you take-even if you think it’s “natural.”
How often should my kidney function be checked if I’m on multiple medications?
At least every 3 to 6 months if you have CKD stage 3 or higher. If you start a new medication, get your eGFR checked before and 1-2 weeks after. If you’re on dialysis, check before each session. Frequent monitoring catches problems early.

Oladeji Omobolaji
January 23, 2026 AT 07:55Man, this hit different. I’m from Nigeria and we don’t have the same access to eGFR tests or fancy apps-just a blood test and a prayer. But I’ve seen cousins on dialysis because they kept taking NSAIDs for back pain. No one told them it could kill their kidneys. This needs to be translated into more languages.
Vanessa Barber
January 23, 2026 AT 09:06So you’re telling me my grandma’s daily ibuprofen for arthritis is slowly killing her kidneys? And her doctor never checked her eGFR? Yeah right. That’s why I stopped trusting doctors after they prescribed metformin to my aunt with a creatinine of 2.1. Classic.
charley lopez
January 23, 2026 AT 11:30The pharmacokinetic implications of reduced glomerular filtration rate on renally excreted pharmaceuticals are profoundly underappreciated in primary care settings. The 42% dosing error rate cited aligns with recent data from the ASHP’s 2023 national audit. Furthermore, the absence of eGFR calculation in 35% of visits reflects systemic gaps in renal risk stratification protocols.
dana torgersen
January 23, 2026 AT 15:36Okay… so… like… eGFR isn’t just creatinine? Wow. I thought they were the same thing… and I’ve been taking metformin for 7 years… and I didn’t know… I mean… what if…? I mean… like… what if I’m already…? I mean… I’m not saying I’m gonna panic… but… I’m gonna panic…
Andrew Smirnykh
January 25, 2026 AT 01:37It’s interesting how this mirrors global disparities. In the U.S., we have apps and FDA tools-but in many places, even basic creatinine tests are expensive. The real issue isn’t just dosing-it’s access. If we can’t measure kidney function, we can’t adjust meds. The solution isn’t just education-it’s equity.
Kerry Evans
January 26, 2026 AT 11:03Look, I’ve been in this game for 20 years. I’ve seen patients die because someone gave them Bactrim with an ACE inhibitor. I’ve seen glyburide cause comas. And you know what? Most of the time, the doctors didn’t even know the guidelines had changed since 2012. This isn’t about patients being dumb-it’s about the system being broken. And now we have AI tools like KidneyIntelX? Great. But if the doctors won’t use them, what’s the point? You can’t fix ignorance with technology if the people holding the levers refuse to learn.
I’ve had patients come in with 14 meds on their list. I ask, "Do you know why you’re taking each one?" Half can’t answer. And the rest say, "My last doctor said to keep taking it." That’s not compliance. That’s negligence. And the system rewards it.
People talk about "patient empowerment" like it’s a magic bullet. But when your doctor dismisses you because you’re "just a patient," no app is going to save you. You need an advocate. You need someone who knows the names of the drugs, the half-lives, the renal clearance thresholds. And if you don’t have that person? You’re one ibuprofen away from dialysis.
I’m not angry. I’m just tired. We’ve had the data for decades. We’ve had guidelines since 2002. And yet, here we are. Still losing people to preventable toxicity. And the worst part? The pharmaceutical companies know. They know the risks. They just don’t care until the FDA slaps them with a $2.5 million fine.
So yeah. Ask your doctor. Bring your list. Use the app. But don’t stop there. Push. Demand. Follow up. Because if you don’t, someone else will die quietly-and no one will notice until it’s too late.
Anna Pryde-Smith
January 27, 2026 AT 00:09MY DAD DIED BECAUSE OF THIS. HE TOOK IBUPROFEN FOR HIS ARTHRITIS. HIS CREATININE WAS 2.8. NO ONE TOLD HIM. NO ONE CHECKED. HE WAS ON 11 MEDS. HE WAS 72. THEY SAID IT WAS "HEART FAILURE." IT WASN’T. IT WAS DRUG TOXICITY. I’M STILL ANGRY. AND I’M STILL SCARED.
Dawson Taylor
January 27, 2026 AT 09:05The kidney’s role as a pharmacokinetic gatekeeper is both elegant and fragile. Its capacity for adaptation is finite. When that threshold is breached, the consequences are not merely clinical-they are existential. The data presented here is not novel. It is corroborated. The failure lies not in knowledge, but in implementation.
Sallie Jane Barnes
January 28, 2026 AT 06:54You are not alone. I’ve been there-watching my mom’s eGFR drop after a new antibiotic. I printed the FDA dosing chart, highlighted every med, and walked into her appointment with my own notes. She cried when the doctor said, "You’re right. We missed this." Don’t wait for them to catch up. Be the one who knows. Be the one who asks. Your voice is your shield.