Mirabegron Pregnancy Risk Checker
How This Tool Works
This tool provides a personalized assessment of Mirabegron safety based on the latest clinical evidence and regulatory guidance. Your results will reflect:
- Pregnancy trimester
- Pre-existing health conditions
- Overactive bladder symptom severity
Note: This tool provides general guidance only. Always consult your healthcare provider for personalized medical advice.
Your Pregnancy Profile
Your Risk Assessment
Risk Factors Analysis
Expert Guidance
Important: This assessment is for informational purposes only. Always consult your healthcare provider for personalized medical advice.
When you discover you’re expecting, every medicine you’ve taken suddenly becomes a question mark. Mirabegron pregnancy safety is one of those questions that pops up fast, especially for women managing overactive bladder (OAB). Below you’ll find a plain‑spoken rundown of what the evidence says, which health agencies think, and how to make the right call with your OB‑GYN.
Key Takeaways
- Human data on Mirabegron use in pregnancy are limited; most guidance relies on animal studies and regulatory classification.
- Regulators label Mirabegron as Category C (FDA) or Risk to the fetus cannot be excluded (EMA), meaning benefits must outweigh potential risks.
- Common side‑effects (high blood pressure, urinary retention) can complicate pregnancy and should be monitored.
- First‑line treatment for OAB in pregnancy usually shifts to behavioral therapy; antimuscarinic drugs like Oxybutynin are considered only if symptoms are severe.
- If you’re already on Mirabegron when you discover you’re pregnant, do not stop abruptly-talk to your provider about tapering or switching.
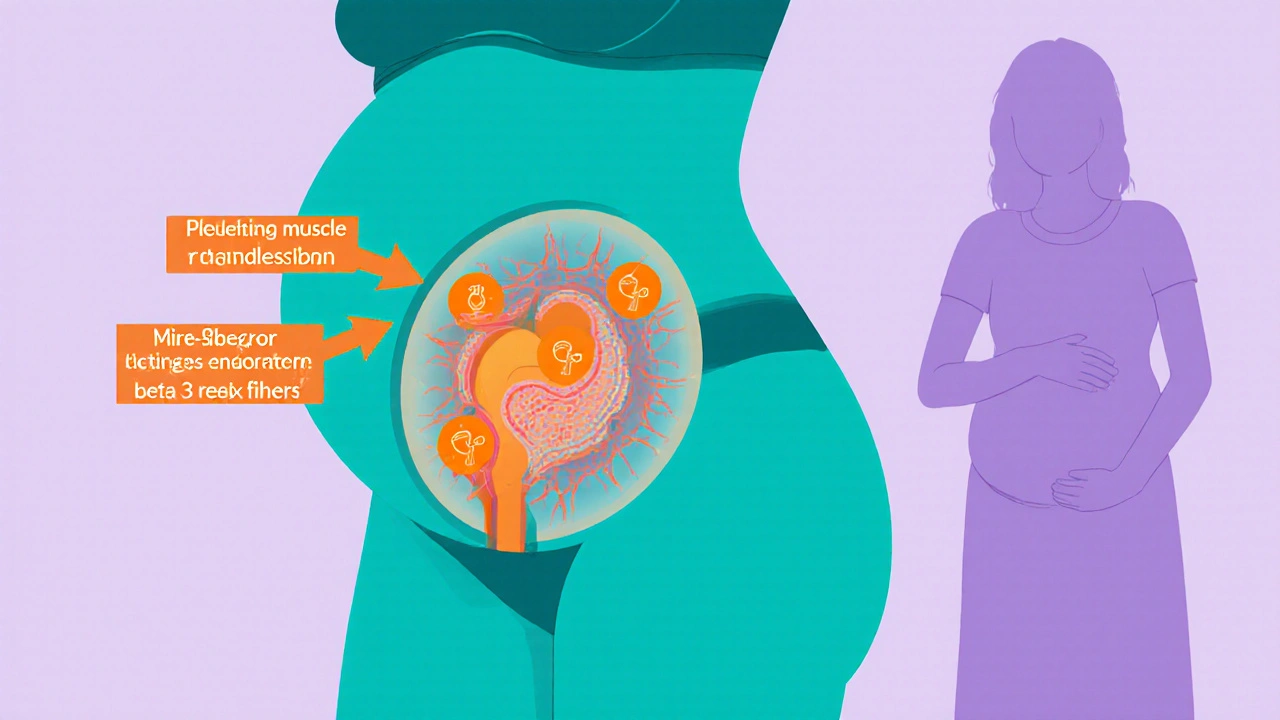
Mirabegron is a beta‑3 adrenergic agonist prescribed to relax the bladder’s detrusor muscle, relieving urgency and frequency in overactive bladder. It was approved in the U.S. in 2012 and quickly became a favorite for patients who couldn’t tolerate anticholinergic side‑effects.
What Is Overactive Bladder and Why Mirabegron Is Used
Overactive bladder (OAB) is a symptom complex-urgency, frequency, nocturia, and sometimes urge incontinence-without an obvious infection or obstruction. In pregnancy, the growing uterus puts pressure on the bladder, often worsening OAB. Lifestyle tweaks (fluid timing, pelvic floor exercises) are first‑line, but many women need meds for relief.
Traditional OAB meds are antimuscarinics (e.g., Oxybutynin, Tolterodine). They block muscarinic receptors in the bladder but can cause dry mouth, constipation, and, importantly for pregnant women, limited data on fetal safety. Mirabegron offers a non‑anticholinergic route, acting on the beta‑3 receptors that control bladder relaxation.
How Mirabegron Works - A Simple Breakdown
Mirabegron binds to beta‑3 adrenergic receptors on the detrusor muscle. Activation triggers a cascade that increases cyclic AMP, leading to muscle relaxation during the filling phase of the bladder cycle. This reduction in involuntary contractions eases urgency and frequency.
Because it doesn’t interfere with acetylcholine pathways, common antimuscarinic side‑effects are largely avoided. However, Mirabegron can raise systolic blood pressure and cause mild tachycardia-effects that need extra scrutiny when you’re pregnant.
Pregnancy Safety Data - What the Numbers Show
Human studies on Mirabegron in pregnancy are sparse. The largest data set comes from post‑marketing surveillance, which has recorded Pregnancy outcomes for roughly 180 women exposed during the first trimester. No clear pattern of major malformations emerged, but the sample size is too small for definitive conclusions.
Animal studies provide the bulk of the evidence. In rats, doses up to 10‑fold the human maximum did not cause teratogenic effects, but higher doses led to fetal growth restriction and reduced ossification. In rabbits, similar high doses produced increased fetal mortality. Regulatory bodies interpret these findings as “potential risk at high exposure,” prompting a cautious stance.
Both the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA) classify Mirabegron as Category C (FDA) and “Risk to the fetus cannot be excluded” (EMA). In practice, this means the drug should only be used if the potential benefit justifies the possible risk.
Regulatory Perspective - FDA, EMA, and National Guidelines
The FDA’s Pregnancy and Lactation Labeling Rule (PLLR) requires a detailed risk summary, data, and clinical considerations. For Mirabegron, the label notes the lack of well‑controlled studies and advises consultation with a specialist before prescribing to pregnant patients.
The EMA’s Committee for Human Medicinal Products (CHMP) echoes the caution, recommending that Mirabegron be avoided in the first trimester unless no alternative exists. Some national obstetric societies (e.g., Royal College of Obstetricians and Gynaecologists in the UK) follow the same line, suggesting behavioral therapy first and reserving medication for refractory cases.
Potential Risks and Side‑Effects Specific to Pregnancy
- Blood pressure elevation: Pregnancy already challenges cardiovascular regulation; uncontrolled hypertension can impact placental perfusion.
- Urinary retention: Although rare, retention can lead to infections, which are more concerning in pregnancy.
- Fetal growth restriction: Animal data hint at this risk at high exposures; clinicians monitor fetal growth via ultrasound if the drug is continued.
- Limited long‑term data: No robust studies track neurodevelopmental outcomes after in‑utero exposure.
Alternatives for Overactive Bladder During Pregnancy
When Mirabegron isn’t a clear choice, doctors turn to non‑pharmacologic measures:
- Timed voiding and fluid management.
- Pelvic floor muscle training (Kegel exercises).
- Bladder training with gradual increase in inter‑void intervals.
- Acupressure or acupuncture - some small trials suggest modest relief.
If medication becomes unavoidable, antimuscarinics are the next option. Below is a quick safety snapshot.
| Medication | Class | Regulatory Pregnancy Category | Key Concerns |
|---|---|---|---|
| Mirabegron | Beta‑3 adrenergic agonist | FDA C / EMA Risk cannot be excluded | Blood pressure rise, limited human data |
| Oxybutynin | Antimuscarinic | FDA C / EMA Risk cannot be excluded | Dry mouth, constipation, possible fetal heart effects |
| Tolterodine | Antimuscarinic | FDA C / EMA Risk cannot be excluded | Similar anticholinergic profile, limited data |

Practical Guidance for Expecting Mothers on Mirabegron
If you’re already taking Mirabegron and discover you’re pregnant, here’s a step‑by‑step plan:
- Don’t panic and don’t stop the drug abruptly. Sudden withdrawal can cause rebound urinary urgency.
- Schedule a prenatal appointment with both your OB‑GYN and urologist. A joint decision ensures bladder symptom control while protecting the baby.
- Ask for a blood pressure check. If you have pre‑existing hypertension, the clinician may lower the dose or switch.
- Consider a gradual taper. Some providers reduce the dose by 25 % every two weeks while monitoring symptoms.
- Explore non‑drug options. Pelvic floor physiotherapy can often replace the medication entirely by the second trimester.
- If medication continues, plan extra fetal growth scans. Ultrasound at 20 weeks and 32 weeks can catch growth restriction early.
All decisions should balance your quality of life with fetal safety. Remember, urinary urgency that disrupts sleep can affect maternal health, so don’t dismiss symptoms as “just part of pregnancy.”
Breastfeeding Considerations
Mirabegron does appear in breast milk in trace amounts (approximately 0.3 % of the maternal dose). The limited data suggest it’s unlikely to cause harm to a nursing infant, but the manufacturer advises caution. If you plan to breastfeed, discuss timing of doses and possible temporary weaning with your pediatrician.
Frequently Asked Questions
Is Mirabegron safe to take during the first trimester?
Evidence is limited, and regulators place it in Category C, meaning it should only be used if the benefit outweighs potential risk. Most clinicians prefer to avoid it in the first trimester unless symptoms are severe and no other options work.
Can Mirabegron cause birth defects?
Animal studies at high doses showed growth restriction and skeletal changes, but human data have not identified a consistent pattern of major malformations. The risk, however, cannot be ruled out, which is why caution is advised.
What should I do if I’ve already been taking Mirabegron and just found out I’m pregnant?
Contact your healthcare provider right away. Do not stop the medication abruptly. Your doctor may suggest a dose reduction, a switch to an alternative, or added monitoring such as blood‑pressure checks and fetal growth ultrasounds.
Are there any non‑drug strategies that work as well as Mirabegron?
Behavioral therapies-timed voiding, bladder training, and pelvic‑floor exercises-are first‑line and often provide substantial relief. Adding a physiotherapist who specializes in pelvic health can boost results without medication.
Can I breastfeed while on Mirabegron?
Small amounts of the drug have been detected in breast milk, but no adverse effects have been reported in infants. Discuss with your pediatrician; some choose to continue, others pause breastfeeding for a short period after a dose.
Bottom line: Mirabegron isn’t outright banned in pregnancy, but the data aren’t robust enough to call it “completely safe.” Work closely with your care team, keep an eye on blood pressure, and explore non‑pharmacologic options whenever possible. Your peace of mind-and your baby’s health-depend on a balanced, well‑informed approach.


Caleb Clark
October 22, 2025 AT 16:20Hey there, future mom! I get how scary it can feel when you see a new med name like Mirabegron pop up on your chart, but let me walk you through why staying calm and staying informed is the best move you can make for you and your baby.
First off, the drug is in that Category C bucket, which means the studies aren't definitive, but it isn't automatically a no‑go either.
What the FDA and EMA are telling us is that the potential benefits must outweigh the potential risks – that's a classic risk‑benefit dance you and your doc will do together.
One big thing to watch is blood pressure – Mirabegron can give it a little nudge, and during pregnancy that can be a bigger deal than usual.
If you're already on it when you find out you're pregnant, do NOT just drop it like a hot potato; a sudden stop can cause a rebound of those pesky urgency symptoms.
Instead, talk to your OB‑GYN and a urologist, and they might suggest a gentle taper – maybe cut the dose by a quarter every two weeks while keeping an eye on how you feel.
Meanwhile, there are non‑drug options that are surprisingly effective: timed voiding, pelvic floor exercises, and even some acupuncture sessions have shown promise.
These strategies can often let you ditch the med altogether by the second trimester, which is great for peace of mind.
Don't forget regular blood pressure checks – a quick cuff reading at each prenatal visit can catch any rise early and keep the placenta happy.
If the doc decides the med is still needed, they’ll likely schedule extra fetal growth ultrasounds around 20 and 32 weeks to monitor the baby's size.
Remember, untreated overactive bladder can mess with sleep and overall wellbeing, so treating the symptoms is also a part of caring for the baby.
In the end, it's all about a balanced approach: you deserve relief, and the baby deserves safety – the best team to achieve that is you and your healthcare crew.
Stay proactive, ask all the questions, and keep that positive mindset – you've got this!
And if you ever feel overwhelmed, just take a deep breath and remember that many moms have navigated this path before you.
Oliver Johnson
October 29, 2025 AT 10:58Mirabegron? Really? The government wants you drinking sweet tea while they shove this ‘Category C’ miracle pill on you – it’s just another way to keep us dependent on Big Pharma!
Taylor Haven
November 5, 2025 AT 06:36Listen, the pharmaceutical lobby has been quietly funding shadow studies for years, and what we’re seeing is a classic case of data suppression; the fact that only 180 pregnancies are reported isn't coincidence, it's a carefully curated narrative to keep the public in the dark.
Every time a new drug lands in the market, the regulators issue a vague Category C label, which is essentially a get‑out‑of‑jail free card for any company that wants to profit off pregnant women.
The animal studies show fetal growth restriction at high doses, yet those results get buried under glossy brochures promising “relief” for overactive bladder.
What they don't tell you is that the increased blood pressure side‑effect can exacerbate pre‑eclampsia, a leading cause of maternal mortality, especially in underserved populations.
And let's not ignore the subtle neurodevelopmental risks that never show up in short‑term follow‑ups but could manifest later in childhood.
Trust me, the silence on long‑term outcomes is a red flag – the industry knows they can’t ethically test on pregnant humans, so they hide behind animal models and vague warnings.
We need more transparent registries, not just post‑marketing surveillance that captures a handful of cases.
The system is rigged to prioritize profit over mother‑baby health, and it’s time we call that out.
Sireesh Kumar
November 12, 2025 AT 02:14Alright, let me break it down with a little drama – imagine you're juggling a kettle of boiling water while trying to keep your phone on silent. That's kinda what starting a med like Mirabegron in the first trimester feels like.
First, the bodily changes in pregnancy already increase bladder pressure; add a beta‑3 agonist and you might think you're easing the load, but you could be turning up the pressure on your cardiovascular system.
Now, the data – we have a tiny handful of human cases, and those are like trying to read a novel through a keyhole. Animal studies are more robust, showing high‑dose skeletal issues; but low‑dose? Still a mystery.
What I love to see is the push for non‑drug approaches – timed voiding, pelvic floor physiotherapy, even yoga for pelvic stability. Those methods are drama‑free and cost‑effective.
If you absolutely must consider meds, a slow taper while monitoring blood pressure every week is the safest route – think of it as a gentle dimmer switch, not a sudden blackout.
And, just a heads‑up, if your doctor suggests a switch to an antimuscarinic, remember those come with their own side‑effects like dry mouth – it's a trade‑off circus.
Bottom line: keep the drama on the stage, not in your uterus.
Gary Marks
November 18, 2025 AT 21:52Alright, strap in because this is where the rubber meets the road. Mirabegron gets a glossy label, but the reality is a mess of half‑baked studies and corporate spin. The drug’s ability to jack up systolic pressure is not a trivial footnote; it’s a potential ticket to preeclampsia, a condition that can turn a pregnancy into a race against time. The post‑marketing data – a measly 180 cases – is laughably insufficient to claim safety, yet it’s paraded as “no major malformations observed.” That’s cherry‑picking at best. Moreover, the animal data screaming about fetal growth restriction and skeletal issues at high doses are shoved into the footnotes while the marketing teams blast the “first‑line alternative to anticholinergics” mantra. Non‑pharmacologic measures like bladder training and pelvic floor therapy are not just polite suggestions; they’re underutilized weapons that could spare countless moms the gamble of a drug with unknown long‑term neurodevelopmental effects. If you’re pregnant and feeling the urge to start this medication, demand a plan: regular blood pressure monitoring, extra ultrasound scans, and a clear taper strategy. Otherwise, you’re basically handing over your baby’s safety to a company that makes a profit from uncertainty. In short, the drug is a gamble, and the odds are stacked against you unless you have no other recourse.
Vandermolen Willis
November 25, 2025 AT 17:31Hey, I get the concerns – it’s a lot to take in. If you decide to stick with Mirabegron, just keep those blood pressure checks regular and maybe add an extra ultrasound for peace of mind. 😊
Mary Keenan
December 2, 2025 AT 13:09This drug is unnecessary.
Holly Green
December 9, 2025 AT 08:47Choosing unnecessary medication during pregnancy compromises both mother and child; it's simply not worth the risk.
Craig E
December 16, 2025 AT 04:25When evaluating Mirabegron, it is essential to balance the pharmacodynamic benefits against the physiological alterations of gestation. The drug's beta‑3 agonism offers a novel mechanism distinct from antimuscarinics, potentially mitigating classic anticholinergic side‑effects. However, its propensity to elevate systolic pressure warrants vigilant monitoring, especially given the hemodynamic shifts inherent to pregnancy. The paucity of robust human teratogenic data places a greater onus on clinicians to employ shared decision‑making, integrating patient values with the limited evidence. Non‑pharmacological interventions remain the cornerstone of management, and they should be thoroughly trialed prior to pharmacotherapy. Should Mirabegron be deemed indispensable, a structured plan encompassing incremental dosing, regular blood pressure assessment, and serial fetal growth ultrasounds is advisable. Ultimately, the principle of 'first, do no harm' should guide therapeutic choices in this delicate context.
Marrisa Moccasin
December 23, 2025 AT 00:03Wow!!! So many technical terms-do you really think the average mom can parse this?!!
And why does everyone act like the drug is either a miracle or a death sentence???
We need clear, honest info, not this corporate‑speak!!!
Seriously, just give us the facts, plain and simple.
Ritik Chaurasia
December 29, 2025 AT 19:42From a cultural perspective, many communities still rely on herbal remedies and traditional pelvic exercises for bladder control during pregnancy, which can be both effective and less stigmatized than taking a prescription like Mirabegron.
Kelli Benedik
January 5, 2026 AT 15:20Oh my gosh, the drama of deciding on a medication during pregnancy is like a soap opera! One minute you’re hopeful, the next you’re terrified that a tiny pill could change your baby’s destiny.
Everyone’s opinions are flying like fireworks, and the stakes feel sky‑high.
But remember, you’re the star of this story, and you get to write the ending – with a little help from your doctor, a dash of research, and maybe a sprinkle of instinct.