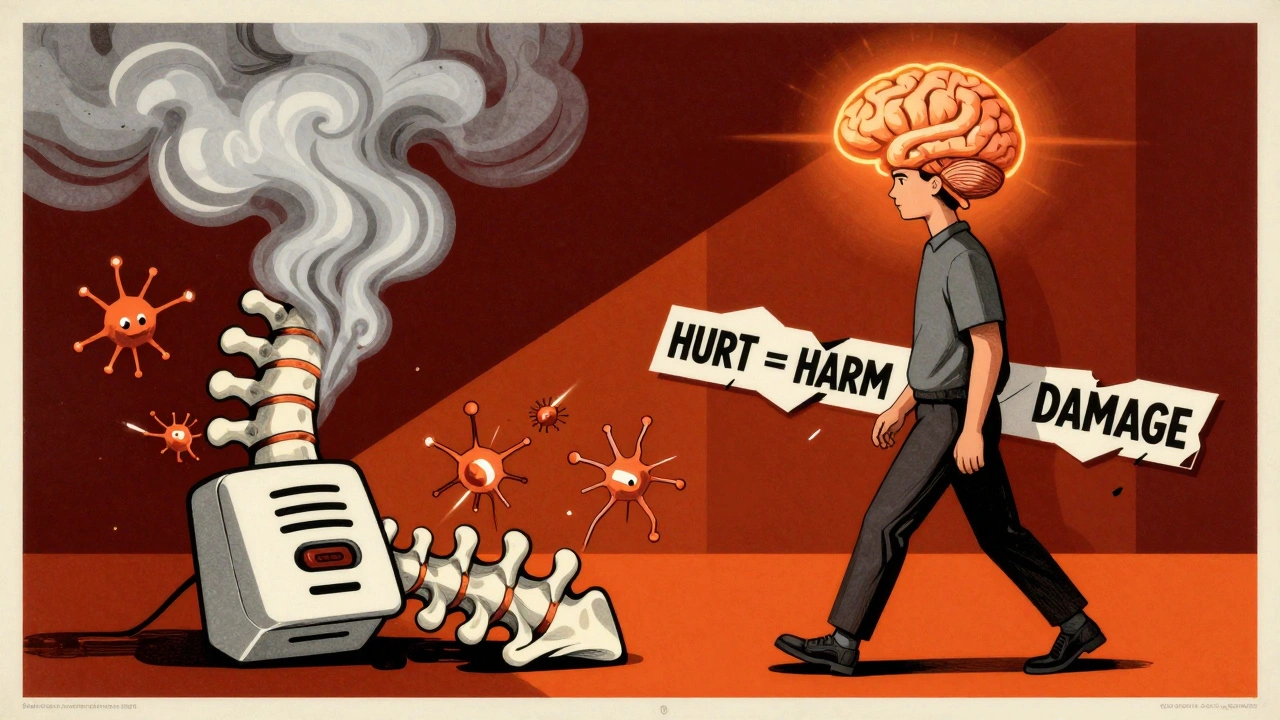
For years, people with chronic pain were told their pain meant damage. A herniated disc. Arthritis. Tendon wear. The message was simple: hurt = harm. But what if that’s not true? What if your pain isn’t a warning light for broken tissue, but a loud alarm system that’s gone off in the wrong room? This is the core idea behind Pain Neuroscience Education - or PNE - and it’s changing how thousands of people live with pain every day.
Why Your Pain Doesn’t Always Mean Damage
Think of your nervous system like a smoke alarm. If there’s a real fire, it goes off. That’s good. But what if the alarm goes off because you burnt toast? Or because dust got in the sensor? That’s not a fire - but the alarm doesn’t know that. It just reacts. Your pain system works the same way. In chronic pain, the nervous system becomes hypersensitive. It’s not that your back is more damaged than it was five years ago. It’s that your brain has learned to interpret even small signals - a stretch, a step, a change in weather - as dangerous. This is called central sensitization. It’s not imaginary. It’s real biology. Brain scans show increased activity in areas that process threat, fear, and emotion when someone with chronic pain moves. The body isn’t broken. The alarm is stuck on high. Traditional pain education focuses on anatomy: “Your L4-L5 disc is bulging.” “Your knee cartilage is worn.” But that kind of talk often makes pain worse. It tells people: move carefully, avoid activity, something is broken. That’s fear-avoidance. And fear-avoidance leads to stiffness, weakness, and more pain - not because the tissue got worse, but because the nervous system got more scared.What Pain Neuroscience Education Actually Does
PNE flips the script. Instead of telling you your body is damaged, it tells you your nervous system is overprotective. It explains how pain is a protective output from your brain - not a direct measurement of tissue damage. It uses simple metaphors, diagrams, and stories to help you understand:- How nerves can become more sensitive over time (peripheral and central sensitization)
- How stress, sleep, emotions, and past experiences all influence pain
- How your brain can change - and how that change can go both ways (neuroplasticity)
- Why movement is safe, even when it hurts
How It’s Done - And Who Does It
PNE isn’t a one-size-fits-all lecture. It’s a conversation. A skilled practitioner - usually a physical therapist, occupational therapist, or pain psychologist - sits with you. They ask questions. They listen. Then they explain pain in a way that makes sense to you. Some use the “Explain Pain” model by David Butler and Lorimer Moseley. They compare the nervous system to a car alarm that’s too sensitive. Others use Adriaan Louw’s approach, which ties pain to the body’s threat system - like a soldier on high alert after too many false alarms. Sessions are usually 30 to 45 minutes. They happen early - often within the first three visits. And they’re rarely done alone. PNE works best when it’s paired with movement. You don’t just learn about pain. You start moving again - slowly, safely, confidently - while understanding that pain doesn’t mean harm.
What the Science Says About PNE vs. Other Approaches
Compare PNE to traditional biomedical education - the kind that says “rest, avoid, protect.” A 2022 review found PNE improved disability scores by 4.7 points on a standard back pain scale. Traditional education? Only 1.2 points. That’s a four-fold difference. When PNE is added to regular physiotherapy, pain reduction jumps from 5.3 points to 10.8 points on a 100-point scale. That’s nearly double the benefit. Even against placebo education - where patients get generic advice like “stay active” without the science - PNE cuts pain catastrophizing by 35% more. And unlike opioids, it doesn’t cause drowsiness, dependence, or overdose risk. But PNE isn’t magic. It doesn’t work for everyone. It’s least effective for acute pain - like after surgery - where actual tissue damage is the main driver. It’s also harder for people with low health literacy or severe cognitive impairment. If you can’t follow the metaphor of a smoke alarm, the lesson won’t stick.Real Stories - What Patients Say
On Reddit’s chronic pain community, one user wrote: “After six months of fearing every movement, the smoke alarm metaphor changed everything. I thought my back was falling apart. Turns out, it was just scared. I’m hiking again. I’ve cut my opioid use by 75%.” Another, a 42-year-old nurse with fibromyalgia, went from six pain pills a day to one every three days after a six-session PNE program combined with graded activity. She didn’t become pain-free. But she became functional. She went back to work. She played with her kids. Not all stories are positive. About 17% of patient reviews complain PNE was “too much science.” Some expected immediate relief. When pain didn’t vanish overnight, they felt let down. That’s a common misunderstanding. PNE doesn’t erase pain. It changes your relationship with it. It helps you stop fighting your body and start working with it.Why Most Clinicians Still Don’t Use It - And How to Get It
Despite the evidence, only 28% of physical therapists in the U.S. feel confident delivering PNE. Why? Training is limited. Most programs don’t teach it. And time is tight. A 45-minute session doesn’t fit neatly into a 15-minute insurance visit. But things are changing. As of 2023, 72% of U.S. physical therapy programs now include PNE in their curriculum - up from just 12% in 2010. Medicare now reimburses for PNE under specific billing codes. And digital tools like the “Pain Revolution” app - downloaded over 186,000 times - are helping patients learn the basics on their own. If you’re struggling with chronic pain and haven’t heard of PNE, ask your provider: “Have you been trained in Pain Neuroscience Education?” If they say no, ask if they can refer you to someone who has. Or look for therapists certified through the International Spine and Pain Institute’s 24-hour course.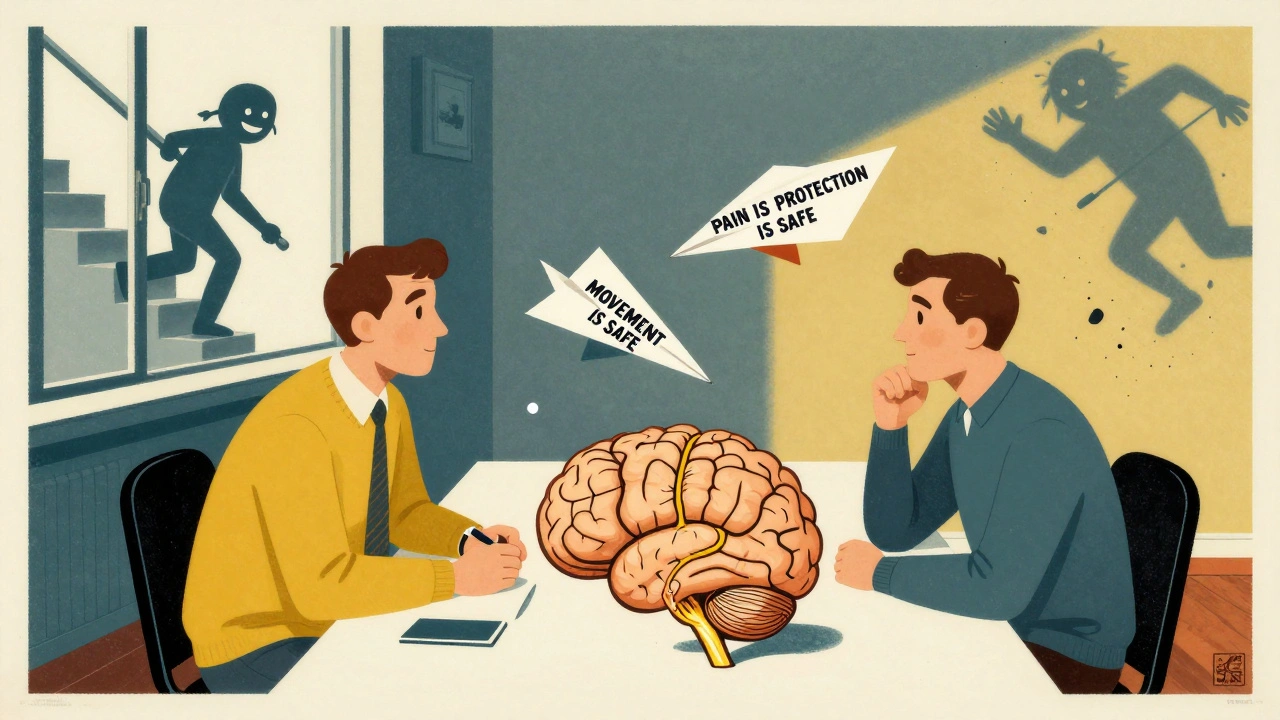
What You Can Do Right Now
You don’t need a clinician to start shifting your pain experience. Here’s what you can try today:- Stop believing pain = damage. Pain is a signal - not a diagnosis.
- Move gently, even if it hurts. Movement teaches your brain that your body is safe.
- Reduce stress. Poor sleep, anxiety, and loneliness all turn up the volume on pain.
- Read The Explain Pain Handbook by Butler and Moseley. It’s simple, clear, and free of jargon.
- Find one thing you stopped doing because of pain - and do it again, slowly. A walk. A stretch. A stair.
What’s Next for Pain Neuroscience Education
Researchers are now testing PNE for acute pain after surgery. Early results suggest it can reduce opioid use and speed recovery. Virtual reality versions are in trials - using immersive stories to teach pain biology. And some clinics are starting to use brain scans to personalize PNE, matching explanations to how each person’s nervous system responds. The bigger shift? Medicine is moving away from “fix the tissue” to “retrain the system.” PNE is leading that change. It’s not about fixing your back. It’s about helping your brain stop overreacting.Frequently Asked Questions
Is pain neuroscience education just for back pain?
No. PNE works for any chronic pain condition where the nervous system has become overprotective - including fibromyalgia, chronic headaches, complex regional pain syndrome, and persistent neck or shoulder pain. It’s not meant for acute injuries like a broken bone or recent surgery, where tissue damage is clearly the main issue.
Will PNE make my pain go away completely?
Not always. But it often makes pain more manageable. Many people don’t become pain-free - they become pain-tolerant. They stop fearing movement. They stop avoiding life. That’s the real win. You might still feel discomfort, but it no longer controls your choices.
Do I need to see a specialist to get PNE?
You don’t need a specialist, but you do need someone trained. Most physical therapists, occupational therapists, and pain psychologists who focus on chronic pain have some PNE training. Ask if they’ve completed a course like the one from the International Spine and Pain Institute. If they haven’t, they may still be able to use the core ideas - just ask them to explain pain as a protective output of the brain, not a damage signal.
Can I do PNE on my own?
Yes - but with limits. Books like The Explain Pain Handbook and apps like Pain Revolution are excellent starting points. But PNE is most powerful when it’s personalized. A trained clinician can adjust the message to your beliefs, fears, and history. Self-learning is a great first step, but working with someone often leads to deeper change.
Why isn’t PNE more widely used if it works so well?
It’s slow to spread. Most clinicians were trained in the old model - pain = damage. Changing that mindset takes time, training, and confidence. Plus, insurance visits are short. Explaining pain neuroscience takes longer than handing out a prescription. But adoption is growing fast. More clinics are offering it. More insurers are paying for it. And more patients are asking for it.

Yasmine Hajar
December 5, 2025 AT 15:33I used to think my chronic back pain meant my spine was falling apart. Then I read about the smoke alarm analogy and it clicked. I stopped avoiding movement and started walking again. Not because it didn't hurt, but because I finally understood that pain isn't a red flag-it's just a noisy alarm. I'm hiking now. I cut my opioids by 75%. This isn't magic. It's biology.
Karl Barrett
December 5, 2025 AT 22:10Central sensitization isn't just a buzzword-it's a neurobiological phenomenon rooted in maladaptive plasticity. The nociceptive threshold is downregulated via NMDA receptor upregulation and glial cell priming in the dorsal horn. What PNE does is recalibrate the threat appraisal network-amygdala, insula, anterior cingulate-by reframing pain as a protective output rather than a sensory input. It's cognitive restructuring at the somatosensory level. The fact that this outperforms pharmacological interventions speaks volumes about the dominance of the biopsychosocial model over the outdated biomedical paradigm.
Jake Deeds
December 7, 2025 AT 16:57Ugh. I hate when people act like pain is 'all in your head' like it's some kind of mindfulness yoga retreat. My pain is real. I've had MRIs. I've had injections. I've had surgery. You can't just 'retrain your brain' and expect a miracle. If my disc is bulging, it's bulging. No amount of metaphors is gonna fix that. This whole PNE thing feels like denial dressed up as science.
val kendra
December 7, 2025 AT 19:27Stop waiting for someone to fix you. You don't need a specialist to start moving again. Even if it hurts. Even if it's slow. Even if it's just one step. Your brain learns safety through action, not words. I've seen people go from bed-bound to hiking trails in 6 months. Not because they got cured. Because they stopped fighting themselves. Pain doesn't vanish. But your power over it? That changes. Just start.
Isabelle Bujold
December 9, 2025 AT 05:41It's fascinating how the concept of central sensitization aligns with the broader understanding of stress physiology-cortisol dysregulation, autonomic nervous system imbalance, and the role of interoceptive awareness. The fact that PNE reduces catastrophizing by over 6 points on standardized scales suggests that the cognitive-emotional architecture of pain is far more malleable than we once believed. And yet, we still treat chronic pain like a mechanical failure. We fix the gear, not the engine. The real revolution isn't in the education-it's in the cultural shift from pathology to process. We need to stop seeing pain as a symptom and start seeing it as a signal of systemic imbalance. That’s the real paradigm shift.
George Graham
December 10, 2025 AT 03:42Just want to say thank you for writing this. I’ve been living with fibro for 12 years. I used to think I was weak because I couldn’t 'push through' the pain. Then I found PNE. It didn’t make the pain go away, but it made me stop hating my body. I started walking again. Not because I had to, but because I wanted to. I’m not cured. But I’m not trapped anymore. That’s worth more than any pill.
John Filby
December 11, 2025 AT 06:56OMG this is so true!! I read the Explain Pain book last year and it literally changed my life 😭 I used to cry every time I bent over. Now I just say 'oh cool, my alarm is loud today' and keep going. Still hurts sometimes but I don't panic anymore. Also, I started doing yoga and my husband says I'm less grumpy. Win win 🙌
Elizabeth Crutchfield
December 11, 2025 AT 07:21i never thought i’d say this but… i think u guys r right. i was so scared to move cause i thought i was breaking myself. now i just go slow. pain still there but it dont own me no more. thx