Probiotic Risk Assessment Tool
Assess Your Risk
This tool helps you understand if probiotics might be safe for you based on your medical condition and immunosuppressant therapy. Always consult your doctor before taking any supplement.
Your Risk Assessment
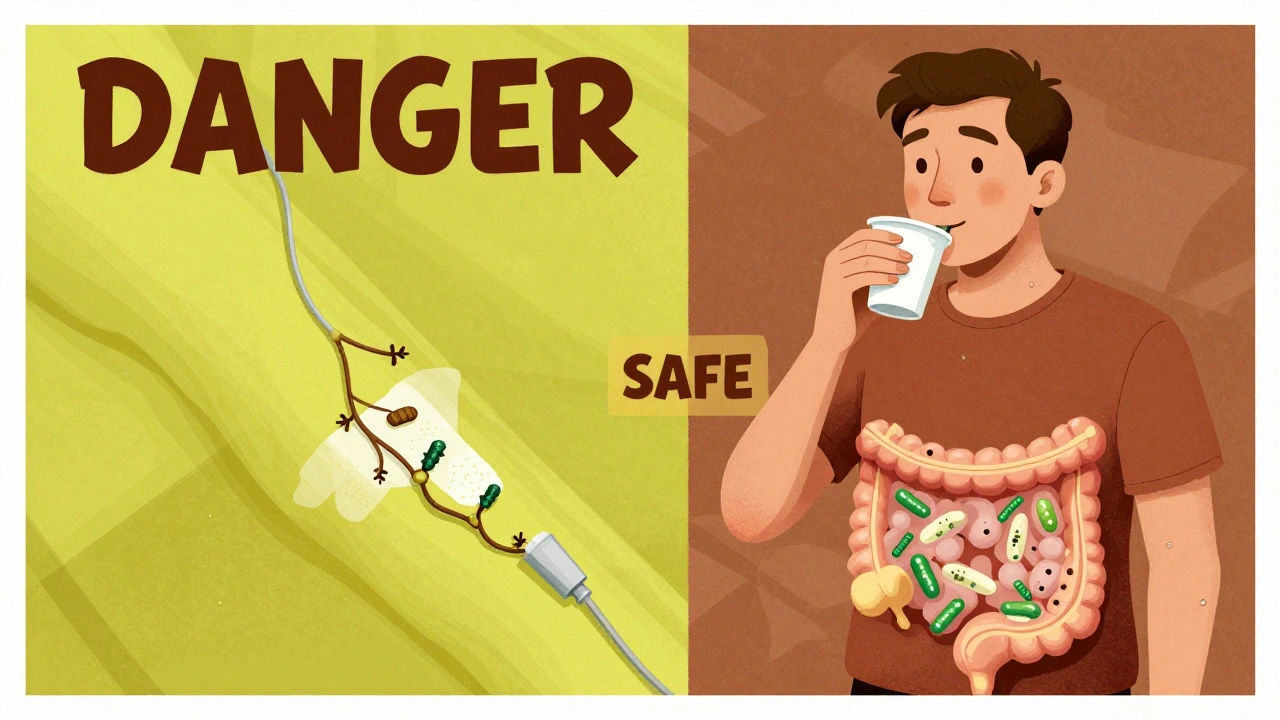
When you're on immunosuppressants-whether after a transplant, for autoimmune disease, or during cancer treatment-your body is already playing defense against its own immune system. Adding probiotics into the mix might sound like a smart move to support gut health, but it can turn into a serious threat. The truth is, what helps a healthy person’s digestion might put someone with a weakened immune system at risk of life-threatening infections.
Why Probiotics Can Be Dangerous for Immunosuppressed People
Probiotics are live microbes-bacteria or yeast-that are meant to support gut balance. Common strains include Lactobacillus a genus of bacteria commonly found in yogurt and supplements, often used to prevent antibiotic-associated diarrhea, Bifidobacterium a genus of beneficial gut bacteria that helps digest fiber and supports immune function, and Saccharomyces boulardii a yeast probiotic used to treat diarrhea, but known to cause bloodstream infections in immunocompromised patients. In healthy people, these microbes stay mostly in the gut and even help block harmful pathogens. But when your immune system is turned down by drugs like tacrolimus, cyclosporine, or rituximab, those same microbes can slip through the gut lining and travel into your bloodstream.This isn’t theoretical. Between 2000 and 2020, 47 documented cases of probiotic-related infections occurred in immunosuppressed patients, according to a study in PMC8706842. Over 80% of those cases happened in people already on immunosuppressants. The most common culprits? Lactobacillus rhamnosus GG and Saccharomyces boulardii. One patient developed sepsis from a probiotic supplement after a kidney transplant. Another developed fungal bloodstream infection from Saccharomyces while on chemotherapy. These aren’t rare outliers-they’re preventable tragedies.
Who’s at the Highest Risk?
Not everyone on immunosuppressants is equally at risk. The danger depends on how weak your immune system is and what kind of drugs you’re taking.- Neutropenia (absolute neutrophil count below 500 cells/µL): This is the biggest red flag. If your body can’t make enough white blood cells to fight infection, even harmless microbes can run wild. Cancer patients in the middle of chemotherapy are especially vulnerable.
- Central venous catheters: If you have a port or PICC line for medication delivery, the risk of bloodstream infection jumps 27% when using Saccharomyces boulardii, according to a 2019 JAMA study. That yeast can cling to the catheter and grow right into your blood.
- Recent organ transplant: The first three months after transplant are the most dangerous. Immunosuppression is at its peak, and your body is still adjusting. A 2021 review found transplant patients in this window had a 4.2 times higher risk of probiotic-related bacteremia.
- Low CD4 count in HIV: If your CD4 count is below 100, your risk of fungal infection from probiotics increases nearly fourfold. Even if you feel fine, your immune system is too compromised to handle live microbes.
On the flip side, people with stable autoimmune conditions on a single drug-like methotrexate or low-dose prednisone-and with normal blood counts may face much lower risk. But even then, caution is needed.
Not All Probiotics Are the Same
A lot of people think “probiotic” means one thing. It doesn’t. Different strains behave differently. One strain might be safe; another could be deadly-even if they’re from the same genus.For example, Lactobacillus rhamnosus GG is one of the most common strains in supplements and has been linked to multiple cases of bacteremia in immunosuppressed patients. But Lactobacillus plantarum 299v, which is approved in Europe for irritable bowel syndrome, has a much cleaner safety record in clinical studies. The same goes for Saccharomyces boulardii: while it helps with diarrhea in healthy people, it’s been tied to 14 documented cases of fungemia since 2020, prompting the FDA to require warning labels on products containing it.
Multi-strain products are riskier than single-strain ones. A 2022 study in Clinical Microbiology and Infection showed single-strain probiotics had 63% less chance of crossing the gut barrier. If you’re immunosuppressed and your doctor still considers probiotics, insist on knowing the exact strain and lot number-not just “Lactobacillus acidophilus.”
When Might Probiotics Be Safe-or Even Helpful?
There’s one group where probiotics have shown clear benefit: liver transplant recipients. A 2022 meta-analysis found they reduced bacterial infections by 34% without increasing serious side effects. That’s the exception, not the rule. For bone marrow transplant patients, the risk outweighs any benefit. For most other groups, the data is too mixed to recommend routine use.Even in liver transplant patients, probiotics should only be used under medical supervision. And they should never be started during the first three months after surgery. Timing matters just as much as the strain.
There’s also emerging research on something called postbiotics inactivated microbial cells and their metabolic byproducts that may offer immune benefits without the infection risk of live probiotics. These aren’t alive, so they can’t cause bloodstream infections. A phase 2 trial in 2024 showed a 40% drop in C. difficile infections in immunosuppressed patients with zero adverse events. This could be the future-but it’s still experimental.
What Doctors Actually Recommend
The Infectious Diseases Society of America (IDSA) breaks risk into four categories:- Category 1 (Highest Risk): Neutropenia under 500, recent stem cell transplant, central lines. Absolute no-go on probiotics.
- Category 2 (Moderate Risk): Solid organ transplant within 3 months, severe autoimmune disease on multiple drugs. Only use after infectious disease consultation.
- Category 3 (Lower Risk): Stable autoimmune disease on one drug, CD4 over 200. Single-strain only, with monitoring.
- Category 4 (Low Risk): No immunosuppression. Standard use is fine.
Major cancer centers in the U.S. avoid recommending probiotics during chemotherapy-induced neutropenia. 87% of them have formal policies against it. Hospitals in the UK and Europe are catching up-62% of U.S. academic centers now have written protocols for probiotic use in immunosuppressed patients, up from 28% in 2018.

What You Should Do
If you’re on immunosuppressants and thinking about probiotics:- Don’t start without talking to your doctor or pharmacist. Even if your supplement says “natural,” it’s not risk-free.
- Ask for strain specifics. If they say “Lactobacillus,” push for the full name: Lactobacillus rhamnosus GG, not just “Lactobacillus.”
- Avoid Saccharomyces boulardii completely. That yeast is the most dangerous probiotic for immunocompromised people.
- Watch for fever. If you develop a fever over 101°F (38.3°C) after starting a probiotic, stop it immediately and get blood cultures done.
- Don’t rely on Reddit or Instagram. Personal stories are compelling but misleading. One person’s “no issues” doesn’t mean it’s safe for you.
If you’re already taking probiotics and have any of the high-risk conditions listed above, stop immediately and call your care team. The risk isn’t worth it.
The Bigger Picture: Why This Is So Hard to Navigate
Probiotics are sold as supplements, not drugs. That means the FDA doesn’t require them to prove safety before they hit store shelves. A bottle labeled “10 billion CFU” could contain any mix of strains, and there’s no guarantee it matches the label. The European Food Safety Authority rejected 95% of probiotic health claims between 2010 and 2020 because the evidence was weak.Meanwhile, the global probiotics market is worth over $52 billion. Companies aren’t incentivized to warn people-they’re incentivized to sell. That’s why so many people think probiotics are harmless. They’re not. Especially not for you.
Insurance rarely covers them. Most cost $30-$50 a month out of pocket. Medicare only covers one prescription probiotic, VSL#3, for a very specific condition called pouchitis. Everything else? You’re on your own.
Final Guidance: Safer Alternatives
If you need gut support while on immunosuppressants, here’s what actually works:- Prebiotic fiber: Foods like oats, garlic, onions, and bananas feed your good bacteria naturally-no live microbes needed.
- Hydration and balanced meals: A healthy gut lining is your best defense. Avoid sugar, processed foods, and alcohol.
- Postbiotics: Watch for emerging products with inactivated bacterial components. These are in early trials but show real promise.
- Regular monitoring: Keep your blood counts and immune markers checked. Your doctor can tell you if your immune system is stable enough to consider anything risky.
The goal isn’t to eliminate gut health-it’s to protect your life. What’s safe for your friend might kill you. Always check with your care team before adding anything new to your regimen.
Can I take probiotics if I’m on prednisone?
It depends. If you’re on low-dose prednisone alone and your immune system is stable (normal blood counts, no recent infections), some doctors may allow a single-strain probiotic like Lactobacillus plantarum 299v. But if you’re on higher doses or combining it with other immunosuppressants, avoid probiotics entirely. Always consult your doctor before starting anything.
Is Saccharomyces boulardii safe for transplant patients?
No. Saccharomyces boulardii has been linked to fatal fungal bloodstream infections in transplant patients, especially those with central lines. The FDA now requires warning labels on all products containing this yeast. It is not safe for anyone on immunosuppressants.
What should I do if I already took probiotics and got sick?
Stop the probiotic immediately. If you have a fever above 101°F (38.3°C), chills, or feel unusually weak, go to the emergency room. Request blood cultures and tell them you’ve been taking probiotics. Early detection saves lives.
Are there probiotics approved for immunosuppressed patients?
No probiotic is officially approved for general use in immunosuppressed patients. VSL#3 is the only one covered by Medicare, and only for pouchitis. Even then, it’s used under strict medical supervision. Most probiotics are sold as supplements, not medications, and lack safety data for this group.
Can I take probiotics after my transplant recovery period?
After the first 3-6 months, if your immune system is stable and you’re on lower doses of immunosuppressants, some doctors may cautiously allow single-strain probiotics. But this is never automatic. You need a formal risk assessment from your transplant team and infectious disease specialist before considering it.
Probiotics aren’t inherently bad-but they’re not harmless either. For someone on immunosuppressants, the stakes are too high to guess. When in doubt, skip it. Your immune system is already working overtime just to keep you alive. Don’t make it fight an invisible enemy you brought in yourself.

alaa ismail
December 2, 2025 AT 13:34Man, I never thought about probiotics being dangerous like this. I’ve been taking that Lactobacillus stuff for years thinking it was just ‘good bacteria.’ Guess I got lucky. Still, wild how something so ‘natural’ can turn into a death sentence if your immune system’s down.
Thanks for laying it out like this. I’m gonna delete my supplement bottle tomorrow.
Allan maniero
December 3, 2025 AT 04:09It’s fascinating, really, how the same biological mechanism that helps a healthy gut thrive can become a Trojan horse in an immunocompromised host. The gut barrier isn’t just a wall-it’s a dynamic, finely tuned interface, and when immunosuppressants dampen the immune surveillance, even benign commensals can translocate.
And let’s not forget the microbiome’s role in immune modulation-it’s not just about pathogens. Probiotics can alter cytokine profiles, dendritic cell activity, even T-reg populations. In someone on tacrolimus, that’s not a minor tweak-it’s a systemic nudge toward disaster. The 47 documented cases? Probably the tip of the iceberg. Most cases go unreported because doctors don’t connect the dots between ‘that probiotic I took’ and ‘sepsis of unknown origin.’
Also, the fact that Saccharomyces boulardii clings to catheters like barnacles? That’s not luck. That’s biofilm formation. We’ve seen it with Candida. Same playbook.
Postbiotics are the future, no doubt. Dead bugs with metabolites? That’s the real ‘smart drug’-no replication risk, no translocation, just signaling molecules that modulate immunity without the chaos. I’m waiting for the first FDA-approved postbiotic for transplant patients. It’s coming.
Sheryl Lynn
December 3, 2025 AT 15:45Oh honey. Let me just say-I’m *so* tired of people treating supplements like vitamins. ‘Natural’ doesn’t mean ‘safe.’ It means ‘unregulated, underfunded, and marketed by people who went to a 3-day webinar on gut health.’
And don’t get me started on Reddit gurus recommending ‘L. plantarum 299v’ like it’s some magical elixir. Do you know how many of those bottles have *zero* live cultures? Or contain *different* strains than what’s on the label? The FDA doesn’t care. The supplement industry is a Wild West carnival with probiotics as the rigged ring toss.
Also, ‘VSL#3’ is covered by Medicare? That’s cute. For one person. For pouchitis. Not for your cousin’s aunt’s friend who ‘feels bloated.’ This isn’t wellness. It’s biohacking gone rogue. And the people who die? They’re just collateral damage in the $52 billion ‘feel-good’ empire.
Eddy Kimani
December 4, 2025 AT 10:13From a clinical microbiology standpoint, the translocation kinetics are critical. Probiotic strains like L. rhamnosus GG express adhesins (e.g., SpaC) that bind to intestinal mucin and epithelial cells-normally benign, but under immunosuppression, they exploit compromised tight junctions via MMP-9 upregulation.
Furthermore, the biofilm-forming capacity of S. boulardii on central venous catheters is mediated by extracellular polysaccharides (EPS) that resist phagocytosis and evade complement-mediated lysis. This isn’t ‘contamination’-it’s opportunistic colonization.
Postbiotics are indeed the next frontier: heat-killed L. casei strains, cell-free supernatants with short-chain fatty acids (SCFAs), and peptidoglycan fragments that activate TLR2 without replication risk. Phase 2 trials show IL-10 upregulation and reduced TNF-alpha-perfect for immunosuppressed hosts.
Bottom line: Don’t ban probiotics. Regulate them. Classify them as Class II medical devices. Require strain-specific FDA clearance for immunocompromised populations. Otherwise, we’re just playing Russian roulette with gut flora.
Chelsea Moore
December 5, 2025 AT 01:42STOP. RIGHT. NOW. I can’t believe people are still even CONSIDERING this!!
YOU’RE ON IMMUNOSUPPRESSANTS. YOU’RE NOT A HEALTHY PERSON. YOU DON’T GET TO ‘TRY THINGS.’
That yeast? That ‘natural’ probiotic? IT’S A FUNGAL TIME BOMB. I’ve seen it. I’ve seen the ICU. I’ve seen the family crying because someone thought ‘a little bacteria couldn’t hurt.’
And now you want to argue about ‘strains’? NO. JUST NO. If you’re on anything that lowers your immune system-STOP. TALKING. TO. STRANGERS. ON. THE. INTERNET.
CALL YOUR DOCTOR. NOT REDDIT. NOT INSTAGRAM. NOT YOUR ‘HEALTH COACH’ WHO SELL’S ‘GUT BALANCE BLENDS.’
YOUR LIFE ISN’T A EXPERIMENT. IT’S A GIFT. DON’T RUIN IT BECAUSE YOU WANT TO ‘FEEL BETTER.’
EVERY. SINGLE. DAY. YOU’RE ALIVE? THANK YOUR IMMUNE SYSTEM. DON’T PISs ON IT WITH PROBIOTICS.
PLEASE. FOR THE LOVE OF GOD. STOP.
John Biesecker
December 5, 2025 AT 05:23Man, this post hit me right in the feels 😔
I’m on low-dose prednisone for my RA and I’ve been taking that ‘gut support’ stuff for months. Thought I was doing good. Now I’m like… did I just put myself in danger? 😳
Thanks for the clarity. Going to toss my bottle today. No regrets, just grateful I read this before something went wrong.
Also, postbiotics sound like sci-fi but I’m here for it 🤖🧬
Maybe one day we’ll have ‘immune-safe’ gut boosters that don’t make your body fight itself. Until then… keep it simple. Oats. Garlic. Water. And listening to your doc, not some influencer with a yoga mat and a supplement brand.
Genesis Rubi
December 7, 2025 AT 04:39Ugh. This is why America’s healthcare is broken. People think ‘natural’ = safe, and then they die because they didn’t trust the system. Meanwhile, China and Germany regulate these supplements like pharmaceuticals. We let anyone sell ‘Lactobacillus’ in a jar and call it medicine.
And now we’re supposed to trust ‘strains’? Like, what? You want me to memorize bacterial taxonomy just to stay alive? No thanks. I’ll take the FDA-approved stuff-when it’s available.
Until then? I’m sticking to food. Real food. Not some fancy powder with ‘10 billion CFU’ printed on it like it’s magic.
And if you’re on immunosuppressants and still taking probiotics? You’re not brave. You’re reckless.
John Morrow
December 9, 2025 AT 00:48The real issue here isn’t probiotics-it’s the commodification of biological complexity. We’ve reduced the human microbiome to a product SKU: ‘Lactobacillus acidophilus + Bifidobacterium lactis.’ As if it’s a laundry detergent that ‘cleans’ your gut.
But the microbiome isn’t a machine. It’s an ecosystem. Introducing exogenous strains into a dysregulated host? That’s not ‘support.’ It’s ecological invasion. And when the host’s immune surveillance is pharmacologically suppressed, the invasive strain doesn’t just colonize-it dominates.
The 47 documented cases? They’re the ones that got caught. How many died quietly without autopsy? How many were mislabeled as ‘sepsis of unknown origin’ because no one thought to ask about supplements?
And the market? $52 billion. That’s not a health industry. That’s a predatory one. They don’t care if you live or die. They care if you click ‘add to cart.’
Postbiotics? Maybe. But until we regulate the entire ecosystem-supplements, labeling, marketing, and medical education-we’re just rearranging deck chairs on the Titanic.