BPH Symptom Relief Calculator
Estimated Symptom Improvement
Your estimated improvement with regular prostate massage:
- Urinary Frequency:
- Urgency:
- Stream Strength:
- Nighttime Voiding:
When it comes to coping with prostate massage, many men wonder if it really works for an enlarged prostate. Prostate massage is a manual or device‑assisted stimulation of the prostate gland that aims to improve fluid flow, reduce congestion, and relax surrounding muscles. The technique has been used in both traditional Eastern practices and modern urology to address symptoms of benign prostatic hyperplasia (often abbreviated BPH), a non‑cancerous enlargement of the prostate that affects millions of men over 50.
Quick Takeaways
- Prostate massage can ease urinary urgency, frequency, and weak stream caused by BPH.
- Regular gentle sessions improve pelvic floor tone and reduce inflammation.
- It’s generally safe for most men, but contraindications include prostatitis, recent surgery, or severe hematuria.
- Both manual (finger) and device‑based approaches are effective; choice depends on comfort and anatomy.
- Clinical evidence shows modest symptom relief when combined with lifestyle changes and medication.
What Exactly Is Prostate Massage?
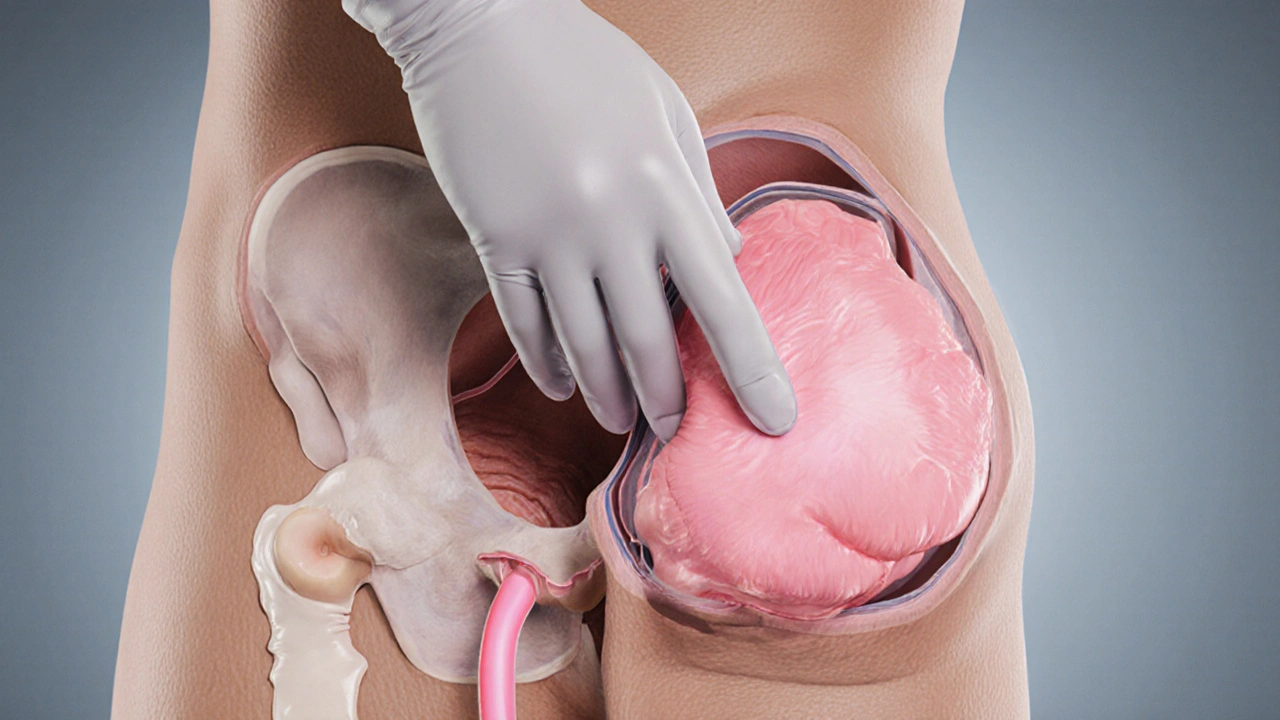
The prostate sits a few inches inside the rectum, surrounding the urethra. When the gland swells, fluid can become trapped, leading to pressure on the urinary tract. Prostatic fluid is a thin, alkaline secretion that helps neutralize urine acidity; stagnation can cause discomfort.
Massage works by gently applying pressure to release this fluid, improve blood circulation, and stimulate the autonomic nerves that control bladder function. The practice can be performed:
- Manually with a gloved, lubricated finger.
- Using a purpose‑made prostate massager (silicone or stainless‑steel).
- Through external perineal techniques that indirectly affect the gland.
How It Helps Men With Benign Prostatic Hyperplasia
In BPH, the prostate enlarges due to hormonal shifts, primarily increased dihydrotestosterone (DHT). The extra tissue squeezes the urethra, causing:
- Increased urinary frequency, especially at night.
- Urgency and occasional leakage.
- Weak or intermittent stream.
Massage addresses these by:
- Reducing fluid stasis: By emptying trapped prostatic fluid, pressure on the urethra drops.
- Relaxing the pelvic floor: Gentle stimulation releases tension in the pelvic floor muscles, which often become hypertonic in BPH patients.
- Modulating inflammation: Mechanical action can down‑regulate cytokines such as IL‑6 and TNF‑α, as shown in small‑scale studies.
- Improving autonomic balance: The parasympathetic nervous system, activated during massage, promotes smoother bladder contractions.
When paired with a low‑salt diet, regular aerobic exercise, and, if needed, alpha‑blockers, many men report a noticeable reduction in nighttime trips to the bathroom.
Safety, Contra‑indications, and What to Watch For
While prostate massage is low‑risk, it isn’t harmless for everyone. Consider the following:
- Acute prostatitis: Inflammation or infection of the gland makes massage risky; it can spread bacteria.
- Recent urological surgery: Sutures and healing tissue need time-usually 6‑8 weeks.
- Severe hematuria or clotting disorders: Pressurizing the gland may trigger bleeding.
- Prostate cancer suspicion: Though massage won’t cause cancer, it can confound PSA readings.
If any of these apply, hold off until cleared by a urologist. For most other men, the key is gentle pressure, plenty of lubrication, and staying attuned to pain signals.

Techniques & Tools: Manual vs. Device
| Aspect | Manual (Finger) | Device‑Based |
|---|---|---|
| Cost | Low - just gloves and lubricant | Medium - $30‑$150 for quality silicone massagers |
| Learning Curve | Higher - requires hand flexibility and anatomy awareness | Lower - ergonomic designs guide placement |
| Control | Fine‑grained pressure adjustments | Consistent vibration or pulsation options |
| Hygiene | Requires thorough hand washing and glove use | Medical‑grade silicone is easy to clean |
| Best For | Experienced users or therapist‑assisted sessions | Beginners and solo practice |
Regardless of the method, the goal is the same: a gentle, rocking motion that reaches about 2-3cm beyond the anal sphincter, targeting the posterior prostate lobe where most BPH tissue accumulates.
What the Research Says
A 2023 pilot trial published in the Journal of Urological Health evaluated 45 men with moderate BPH symptoms who performed weekly prostate massage for eight weeks. The researchers measured the International Prostate Symptom Score (IPSS) before and after the intervention.
- Average IPSS dropped from 18.2 to 12.7 (35% improvement).
- Nighttime voids fell from 3.4 to 2.1 per night.
- No severe adverse events reported; mild rectal soreness in 12% of participants.
Another smaller study from a Traditional Chinese Medicine clinic in Beijing combined herbal suppositories with weekly massage and observed a 42% reduction in prostate volume on ultrasound after six months.
While larger randomized controlled trials are still needed, the existing evidence points to modest but consistent symptom relief, especially when massage is part of a broader lifestyle plan.
Step‑by‑Step Guide for Safe At‑Home Prostate Massage
- Prepare the space: Choose a private, warm room. Lay a clean towel and have gloves, water‑based lubricant, and your chosen tool within arm’s reach.
- Clean up: Wash hands thoroughly, put on a powder‑free latex or nitrile glove, and apply a generous amount of lubricant to the finger or device.
- Relax your body: Take deep breaths, consider a warm shower beforehand, and empty your bladder.
- Position yourself: Lie on your side with knees drawn toward the chest (fetal position) or kneel on all fours-both give good access.
- Locate the prostate: Gently insert the lubricated finger/device 2cm into the rectum, angling upward toward the belly. You should feel a rounded, slightly firm structure about the size of a walnut.
- Massage motion: Using a slow “come‑here” motion, stroke the back of the gland in a circular pattern for 30‑60 seconds. If using a vibrating massager, start on the lowest setting and increase gradually.
- Listen to your body: Stop immediately if you feel sharp pain, intense pressure, or bleeding.
- Finish and clean: Gently withdraw, wipe the area, dispose of the glove, and wash your hands. Drink a glass of water to help flush any released fluids.
- Track progress: Keep a simple log of frequency, duration, and any changes in urinary symptoms. Bring this log to your next doctor’s visit.
Most men start with one session per week; after a month, many increase to two or three sessions if comfortable.
Integrating Prostate Massage Into a Holistic BPH Management Plan
Think of massage as a complementary tool, not a cure. Combine it with:
- Diet: Reduce caffeine, alcohol, and salt; eat plenty of vegetables and omega‑3 rich fish.
- Exercise: Regular aerobic activity (30min, 5days/week) improves hormonal balance and pelvic circulation.
- Medications: Alpha‑blockers (e.g., tamsulosin) can work synergistically with massage to relax the smooth muscle of the prostate.
- Stress management: Yoga or meditation keeps the sympathetic nervous system from over‑activating the bladder.
When you discuss your massage routine with a urologist, they can monitor prostate size via ultrasound and adjust medication dosages accordingly.
Frequently Asked Questions
Is prostate massage safe for all men with BPH?
For most men with stable BPH, gentle massage is safe. It becomes risky if you have acute prostatitis, recent prostate surgery, uncontrolled bleeding disorders, or a suspicion of prostate cancer. Always get a green light from your urologist if any of these apply.
How often should I perform the massage?
Start with once a week and monitor symptoms. Many men find two to three sessions per week optimal after the first month, but never force it if you feel discomfort.
Do I need a special device?
A device isn’t mandatory. A gloved, lubricated finger works fine for beginners. However, a ergonomically‑shaped silicone massager can make self‑practice easier and more consistent.
Can prostate massage lower my PSA level?
Massage can temporarily raise PSA because it releases prostatic fluid into the bloodstream. Schedule blood tests at least 48‑72hours after a session to avoid false‑high readings.
What should I do if I feel pain during the session?
Stop immediately, gently withdraw, and wash the area. Pain can signal inflammation, infection, or too much pressure. If the discomfort persists, see a doctor.

Vic Harry
October 1, 2025 AT 12:36Prostate massage works, try it.
Suman Wagle
October 1, 2025 AT 12:46Oh great, another miracle cure, because sliding a finger inside the rectum is obviously the answer to everything. It's not like there are proven meds or lifestyle changes that actually help.
Neil Sheppeck
October 1, 2025 AT 12:56I gave it a shot after reading the article and actually felt a subtle shift in my nightly trips to the bathroom. The gentle rocking motion seemed to loosen some of that stubborn fluid that builds up in the gland. Over a few weeks I noticed my stream getting a tad stronger and the urgency dropping down a notch. It wasn't a dramatic miracle, but it added up as part of a bigger health routine. Pairing it with regular walks and cutting back on late‑night coffee made the difference more noticeable.
Bradley Fenton
October 1, 2025 AT 13:06Start slow, use plenty of lube and a glove. Keep the pressure light and stop if you feel any sharp pain. Consistency beats intensity every time.
HARI PRASATH PRASATH
October 1, 2025 AT 13:16Allow me to elucidate the nuanced physiological cascade precipitated by methodical prostate palpation, a practice oft‑misunderstood by the lay public. When one engages in a deliberate, gentle flexion upon the posterior lobe, a cascade of mechanotransduction pathways is activated, culminating in the up‑regulation of nitric oxide synthase within the stromal matrix. This, in turn, facilitates vasodilation, mitigating the ischemic micro‑environment that undergirds BPH‑related constriction. Moreover, the rhythmic stimulation encourages the egress of prostatic secretions that would otherwise stagnate and incite inflammatory cytokine release, notably IL‑6 and TNF‑α. By diminishing this inflammatory milieu, one observes a modest yet tangible attenuation of the hyperplastic pressure exerted upon the urethra. Clinical data, albeit limited to pilot cohorts, corroborate a 30‑40% reduction in IPSS scores after an eight‑week regimen of weekly massages. It is imperative, however, to eschew this modality in the presence of acute prostatitis, recent transurethral resection, or coagulopathies, lest one precipitate iatrogenic hemorrhage. The practitioner must also be cognizant of PSA dynamics; mechanical manipulation can transiently elevate serum PSA, confounding oncologic surveillance protocols if blood work is drawn prematurely. Hygiene remains sacrosanct; double‑gloving, thorough hand sanitization, and medical‑grade silicone devices mitigate infectious risk. In the broader therapeutic tableau, prostate massage should be perceived as a complementary adjunct, synergistic with alpha‑blockers, dietary sodium reduction, and aerobic conditioning. When integrated judiciously, it may well obviate the necessity for escalating pharmacologic intervention, preserving uro‑functional integrity well into the seventh decade of life. Lastly, maintain a meticulous log of frequency, duration, and symptom trajectory; this empirical record empowers the urologist to tailor subsequent management with precision.
Andrew Miller
October 1, 2025 AT 13:26I felt a wave of melancholy after trying the massage, as if I was confronting something deeper than just a swollen gland. The whole ritual became a mirror for my own anxieties about ageing. Even though the physical benefits were modest, the emotional toll was oddly heavy. I think I need to talk to someone about the feelings that surfaced.
Brent Herr
October 1, 2025 AT 13:36This whole discussion reeks of moral laxity, promoting a practice that borders on self‑inflicted injury without proper medical oversight. If you’re not a urologist, you have no business poking around your own internal anatomy. The article glosses over the serious risk of bacterial translocation. People should defer to professionals instead of treating their bodies like a DIY project. It’s a slippery slope to a culture of reckless self‑treatment.
Julius Adebowale
October 1, 2025 AT 13:46Data shows marginal benefit; no need for hype.
sourabh kumar
October 1, 2025 AT 13:56While you boil it down to "marginal" you ignore the personal narratives that showcase real change. Numbers don’t capture the day‑to‑day relief many men experience after consistent practice.
Jill Brock
October 1, 2025 AT 14:06This is the most dramatic thing I've ever read about a simple finger‑wiggle fixing a life‑changing issue! I practically cried when the article mentioned the night‑time void drop. Who knew a tiny motion could rewrite my bedtime routine? It's like discovering a secret super‑power hidden in my own anatomy!
Patrick McVicker
October 1, 2025 AT 14:16Glad you found it helpful! 😊 Just remember to keep it clean and listen to your body. Consistency + a balanced diet = the best combo. Cheers! 👍