Don’t Just Take It-Ask About It
You pick up your prescription, grab the pill bottle, and head out. But do you actually know what you’re taking, why, or what might happen if you mix it with your morning coffee or that herbal supplement you’ve been using for years? Too many people treat medications like mystery boxes-pop them, hope for the best, and pray nothing goes wrong. That’s not safety. That’s luck.
Pharmacists aren’t just the people who hand you your pills. They’re trained medication experts, often more accessible than your doctor. In the U.S., 94% of people live within five miles of a community pharmacy. That means your pharmacist is probably closer than your nearest urgent care. And they’re legally required to help you understand your meds. But only if you ask.
What Is This Medicine For, Really?
Start with the basics. Ask: "What is this medication for?" Sounds simple, right? Yet nearly 30% of medication errors happen because patients don’t know why they’re taking something. Maybe your doctor prescribed it for high blood pressure, but you’ve been taking it because you thought it was for "energy." Or maybe it’s an antibiotic you were told to finish, but you’re not sure what infection it’s targeting.
Don’t settle for "it’s for your condition." Ask for clarity: "How will this help me feel better?" or "Is this treating the cause or just the symptoms?" Understanding the purpose helps you track whether it’s working-and when to worry if it’s not.
How and When Do I Take This?
Dosing instructions aren’t just suggestions. They’re science. Take a blood pressure pill with food when it should be on an empty stomach? It might not absorb properly. Take a painkiller at night when it causes drowsiness? That’s fine. Take it in the morning? You might crash at work.
Ask these specific questions:
- Should I take this with food, or on an empty stomach?
- What time of day works best?
- Can I crush, chew, or split this pill?
- Should I avoid driving, alcohol, or sun exposure while taking this?
One patient in a 2022 study missed doses because they didn’t realize their cholesterol medicine had to be taken at bedtime. Another developed stomach bleeding from taking an NSAID with coffee every morning-something the pharmacist could have warned them about in seconds.
What Side Effects Should I Watch For?
All medications have side effects. Some are mild. Others can be dangerous. Ask: "What are the most common side effects?" and "Which ones mean I need to call my doctor right away?"
For example, if you’re on an antidepressant and start feeling unusually agitated or having suicidal thoughts, that’s a red flag. If you’re on a statin and get unexplained muscle pain, that could signal a serious reaction. Pharmacists know which side effects are normal and which are emergencies.
Also ask: "How can I manage the side effects?" Maybe nausea can be eased by taking the pill with a small snack. Maybe dizziness improves after the first week. Knowing this helps you stick with the treatment instead of quitting because you felt awful.
Could This Interact With Anything Else I’m Taking?
This is one of the most overlooked-and dangerous-questions. One in five hospital admissions due to medications happens because of bad interactions. You might not think your fish oil or turmeric supplement matters. But they can.
Ask: "Does this interact with my other prescriptions, over-the-counter meds, vitamins, or herbal supplements?"
One Reddit user discovered their blood pressure medication clashed with hawthorn berry supplements they’d been using for "heart health." Their pharmacist flagged it immediately. Another patient developed serotonin syndrome after combining tramadol with St. John’s Wort-something their doctor never asked about.
Bring a list. Every pill. Every capsule. Every tea. Your pharmacist can spot hidden risks you didn’t even know existed.
What If I Miss a Dose?
Life happens. You forget. You’re traveling. You’re sick. You run out. Instead of guessing what to do, ask: "What should I do if I miss a dose?"
Sometimes you take it right away. Sometimes you skip it. Sometimes doubling up is dangerous. For example, missing a dose of warfarin (a blood thinner) can increase clot risk. Missing a dose of insulin? That’s a medical emergency. But missing one dose of an acne pill? Maybe it’s fine.
Pharmacists can give you a clear, personalized plan. And they can help you set up reminders-phone alerts, pill boxes, even text message systems some pharmacies offer for free.

Is There a Cheaper or Generic Option?
Brand-name drugs can cost 80-85% more than generics. And here’s the truth: generics are required by law to work exactly the same way. Same active ingredient. Same dose. Same safety profile.
Ask: "Is there a generic version available?" If the answer is yes, ask: "Can I switch to it?" Most insurers push generics because they’re cheaper-and you save money without losing effectiveness.
Also ask: "Are there cost-saving programs, coupons, or patient assistance plans?" Many drugmakers offer discounts. Pharmacies sometimes have $4 generic lists. You won’t know unless you ask.
When Will I Start Feeling Better?
Antibiotics? You might feel better in 2-3 days. Antidepressants? It can take 4-6 weeks. Blood pressure meds? You might not feel anything at all-and that’s normal.
Ask: "When should I expect to notice improvement?" and "Will I need tests to check if it’s working?"
Too many people stop taking meds because they don’t feel immediate results. A 2022 Harvard Health report found 68% of patients don’t know when their medication should start working. That leads to unnecessary switches, missed doses, or worse-stopping entirely.
Are There Non-Drug Options?
Not every problem needs a pill. Ask: "Are there lifestyle changes, diet adjustments, or physical therapies that could help?"
For example, someone with early-stage type 2 diabetes might be able to manage it with weight loss and exercise instead of metformin. Someone with mild anxiety might benefit from cognitive behavioral therapy before starting an SSRI.
Pharmacists know what works. They’ve seen what helps patients avoid meds altogether-or use less of them. Don’t assume pills are the only path.
How Do I Know This Is the Right Medication?
Some patients are on multiple drugs. One man in a Brown University case study was taking two different acid-reducing pills-both prescribed by different doctors. His pharmacist caught the duplication. One was enough. The other was risking kidney damage.
Ask: "Is this medication still needed?" or "Could any of my meds be replaced or removed?"
Medication reviews aren’t just for seniors. Anyone on three or more prescriptions should have one at least once a year. Pharmacists can spot duplicates, unnecessary overlaps, or outdated prescriptions.
How Can I Make This Easier to Remember?
Medication non-adherence costs the U.S. healthcare system $300 billion a year. That’s because people forget, get confused, or feel overwhelmed.
Ask your pharmacist: "What tools or systems do you recommend to help me stay on track?"
Some pharmacies offer blister packs with days of the week labeled. Others send text reminders. Some even offer home delivery. Use them. The teach-back method works too: after they explain, say, "So if I miss a dose, I should…" and repeat it back. Studies show this boosts adherence by 40%.
Where Can I Find Reliable Info Later?
Google is full of misinformation. Facebook groups? Even worse. Ask: "Where can I find trustworthy, up-to-date information about this medication?"
Reputable sources include the FDA’s website, MedlinePlus (from the National Library of Medicine), or your pharmacy’s patient portal. Pharmacists can point you to free, accurate materials-no ads, no hype.
What’s Changed Since Last Time?
If you’ve been taking the same meds for years, ask: "Has anything changed with this drug?" New warnings? New interactions? New generics?
Medications get updated. In 2023, the FDA added new safety labels to dozens of common drugs. Your pharmacist tracks these changes. You might not.
How Do I Prepare for My Visit?
Don’t walk in blind. Bring:
- A complete list of everything you take: prescriptions, OTC meds, vitamins, herbs, supplements
- Your insurance card and ID
- Any new symptoms or concerns you’ve had since your last visit
- A notebook or phone to write down answers
Use the FDA’s free "My Medicine Record" form-it’s online and takes five minutes to fill out. It covers 17 key details pharmacists need.
Why This Matters More Than You Think
Pharmacist interventions reduce hospital visits by 33% and prevent 1.5 medication errors per patient admission in hospitals. In community pharmacies, asking just three specific questions cuts medication-related problems by 65%.
And yet, most people don’t ask. A 2022 Consumer Reports survey found 63% of patients felt rushed during pharmacy visits. Average consultation time? Just 2.7 minutes. That’s not enough to cover everything.
So be prepared. Be clear. Be bold. Your pharmacist is there to help. They want you to get better. But they can’t read your mind.
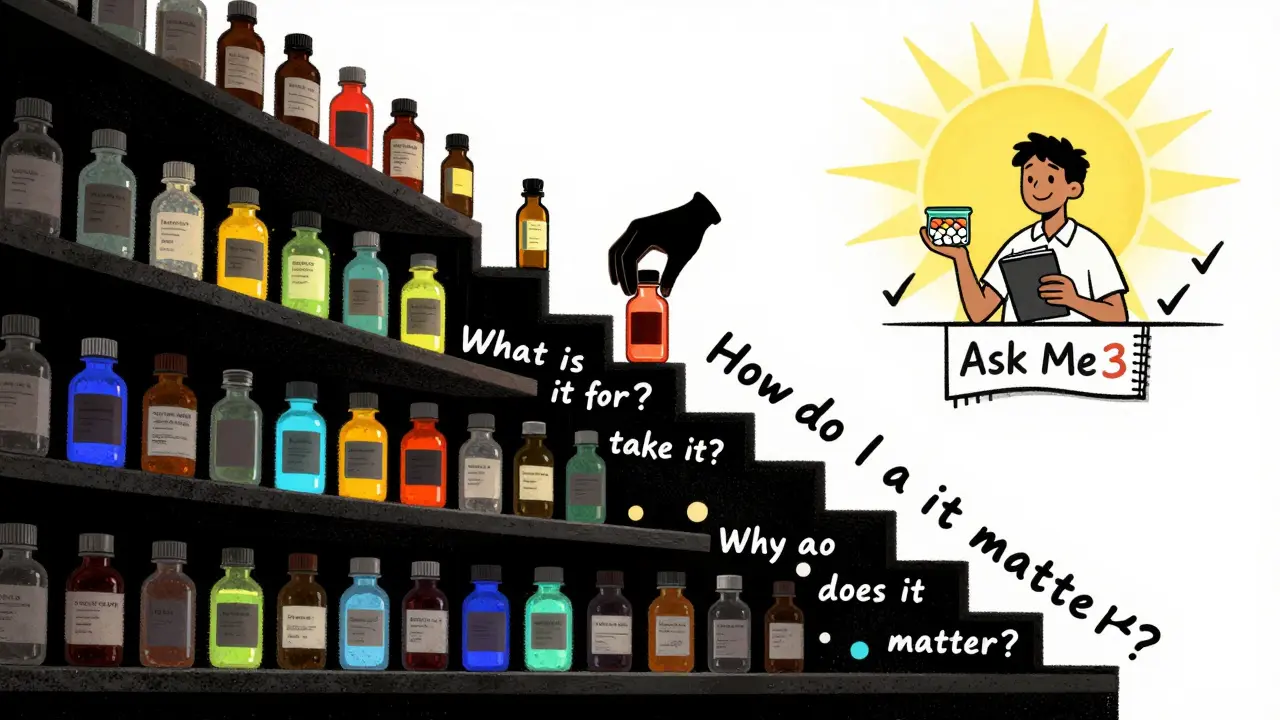
Final Thought: Ask Three Questions
The American Pharmacists Association launched the "Ask Me 3" campaign for a reason. Ask:
- What is my main problem?
- What do I need to do?
- Why is it important for me to do this?
If you ask those three, you’ve covered 90% of what matters. And you’ve just made your healthcare safer, smarter, and more effective.

