Statins are one of the most prescribed drugs in the world. If you’ve been told your cholesterol is too high, there’s a good chance your doctor reached for a statin. And for good reason: these drugs have saved millions of lives. But not everyone tolerates them well. Muscle pain is the most common complaint-and it’s often misunderstood. Some people stop taking them because they think the side effects are worse than the risk of a heart attack. Others push through discomfort, thinking it’s just "part of the deal." The truth? It’s more nuanced than that.
How Statins Actually Lower Cholesterol
Statins don’t just "block" cholesterol like a filter. They work by targeting an enzyme in your liver called HMG-CoA reductase. That enzyme is the main factory for making cholesterol. When statins slow it down, your liver produces less cholesterol. That’s step one. Step two is even smarter: when your liver detects less cholesterol, it pulls more LDL (the "bad" kind) out of your bloodstream to make up the difference. Think of it like a store running low on stock-it starts ordering more from suppliers. Your liver becomes a cholesterol vacuum. On average, statins drop LDL by about 1.8 mmol/L (or 70 mg/dL). That’s a 60% reduction in heart attack risk for most people. High-intensity statins like atorvastatin 40-80 mg or rosuvastatin 20-40 mg can cut LDL by over 50%. Even moderate doses like simvastatin 20-40 mg bring LDL down by 35-45%. But it’s not just about LDL. Statins also reduce inflammation in artery walls, stabilize plaque so it doesn’t rupture, and improve how blood vessels relax. These effects happen even before LDL drops much. That’s why some people feel better within weeks-not because their cholesterol changed, but because their blood vessels started functioning better.The Real Risk: Muscle Pain
Muscle pain is the #1 reason people stop taking statins. But here’s what most don’t know: true muscle damage (rhabdomyolysis) is extremely rare-less than 1 in 10,000 people per year. What’s far more common is something called statin-associated muscle symptoms (SAMS). This includes aches, cramps, stiffness, or weakness, usually in the thighs, shoulders, or back. Studies show 5-10% of people on statins report muscle discomfort. But here’s the twist: in placebo-controlled trials, up to 70% of people who say they had muscle pain on statins had the same pain when they took a sugar pill instead. That suggests a lot of the pain isn’t directly caused by the drug-it’s the fear of the drug, or coincidence, or aging. Still, for the real 5-10%, it’s not trivial. One patient in Edinburgh told me his legs felt like they were filled with lead after six months on simvastatin. He couldn’t climb stairs without stopping. He thought he was just getting older. It wasn’t until he switched to pravastatin that the pain vanished. Pravastatin is less likely to cause muscle issues because it’s processed differently in the body-it doesn’t rely as much on liver enzymes that can build up in muscle tissue.Who’s at Higher Risk for Muscle Pain?
Not everyone is equally likely to get muscle pain from statins. Certain factors raise the risk:- Age over 75
- Small body frame or low muscle mass
- Chronic kidney disease
- Taking other medications like fibrates, cyclosporine, or certain antibiotics
- Genetics-especially a variant in the SLCO1B1 gene, which affects how your body clears simvastatin
- High doses of statins

What to Do If You Have Muscle Pain
Don’t just quit. Don’t suffer silently. Talk to your doctor. Here’s what works:- Check your creatine kinase (CK) levels. If they’re normal and your pain is mild, it’s likely not muscle damage.
- Switch statins. Try pravastatin or fluvastatin-they’re gentler on muscles.
- Reduce the dose. Sometimes 20 mg of atorvastatin works just as well as 40 mg for your risk level.
- Try every-other-day dosing. Some people tolerate this fine, especially with longer-acting statins like rosuvastatin.
- Consider coenzyme Q10. It’s not magic, but some people report less pain after taking 100-200 mg daily. It’s cheap, safe, and worth a try.
Benefits vs. Risks: The Numbers Don’t Lie
Let’s put this in perspective. If you’ve had a heart attack or have diabetes and high cholesterol, taking a statin cuts your risk of another heart attack by about 30%. That’s not a small number. For every 1 mmol/L drop in LDL, you reduce your risk of major vascular events by 22%. That’s proven across 20+ years of research. The risk of serious muscle damage? Less than 0.1%. The risk of liver damage? Even lower. The risk of developing type 2 diabetes? A 9-12% increase-but only in people already at high risk. And even then, the heart protection outweighs the diabetes risk. A 72-year-old man in Glasgow with a history of heart disease and an LDL of 4.2 mmol/L? His chance of dying from heart disease in the next 10 years without a statin is about 25%. With a statin? It drops to 17%. That’s 8 lives saved per 100 people. Meanwhile, maybe one of them gets muscle pain. That’s not a fair trade? I’d argue it’s the smartest choice.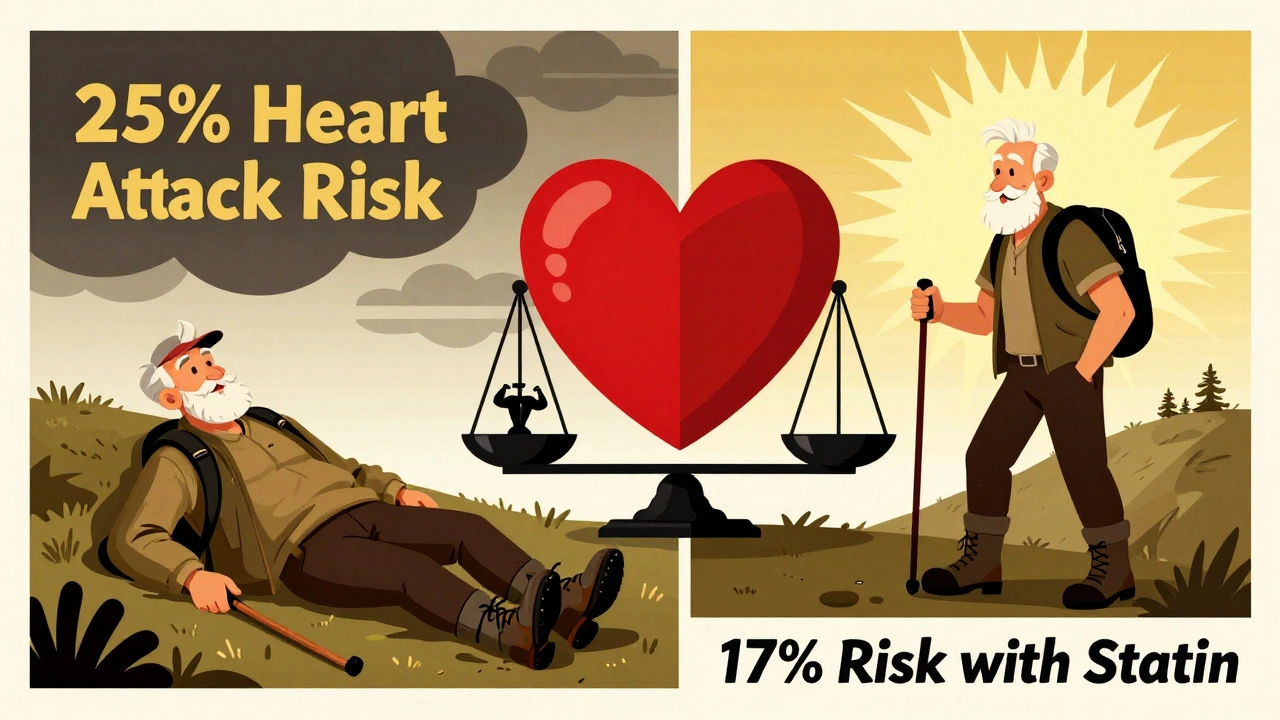
When Statins Aren’t Right for You
There are cases where statins aren’t the best first move:- If you’re young, healthy, and just have mildly high cholesterol-lifestyle changes (diet, walking, weight loss) often come first.
- If you have a history of severe muscle pain on multiple statins, and genetic testing shows SLCO1B1 risk.
- If you’re over 75 with no history of heart disease-benefits are smaller, risks may be higher.
- If you’re pregnant or planning to be-statins are not safe.
What’s Next for Statins?
Researchers are working on smarter versions. One new approach targets only the liver, so the drug doesn’t reach muscle tissue at all. Another is using gene testing to predict who’ll have side effects before they start. Right now, we’re flying blind for a lot of people. But in five years, you might get a simple blood test before your first statin-and know exactly which one will work for you. For now, the message is simple: don’t assume muscle pain means you can’t take statins. Don’t assume you’re fine just because you feel okay. Talk to your doctor. Test your CK. Try a different statin. Adjust the dose. You don’t have to choose between a heart attack and aching legs. There’s a middle ground.Statins aren’t perfect. But for millions, they’re the difference between life and death. And for many others, they’re the difference between living well and being held back by fear.
Do statins really lower cholesterol, or is it just a myth?
Yes, statins lower cholesterol-very effectively. They reduce LDL (bad cholesterol) by 30-60%, depending on the drug and dose. This isn’t theory-it’s backed by decades of clinical trials. The mechanism is well understood: statins block an enzyme in the liver that makes cholesterol, forcing the liver to pull more LDL out of your blood. Studies like the Heart Protection Study and 4S trial show this directly cuts heart attacks and strokes.
Is muscle pain from statins dangerous?
Most muscle pain from statins isn’t dangerous-it’s called myalgia and doesn’t involve muscle damage. But in rare cases, it can lead to rhabdomyolysis, where muscle tissue breaks down and can damage kidneys. That happens in fewer than 1 in 10,000 people per year. If you have severe muscle pain, dark urine, or weakness, get your creatine kinase (CK) levels checked. Normal CK means it’s likely not serious. High CK means you need to stop the statin.
Can I take coenzyme Q10 to prevent muscle pain?
Some people report less muscle pain when taking coenzyme Q10 (CoQ10), but the science isn’t solid. Statins lower CoQ10 levels in the body, and since CoQ10 helps muscles produce energy, it makes sense that supplementing might help. A few small studies show modest benefit, but large trials haven’t confirmed it. Still, CoQ10 is safe and cheap-many doctors recommend trying 100-200 mg daily if you have mild muscle discomfort. Don’t expect miracles, but it’s worth a shot.
Which statin causes the least muscle pain?
Pravastatin and fluvastatin are generally the gentlest on muscles because they’re processed differently in the liver and don’t build up in muscle tissue like simvastatin or atorvastatin. Rosuvastatin can be strong but is often well-tolerated. If you have muscle pain on one statin, switching to another often helps. Many people who quit statins because of pain find relief after switching-sometimes even on the same dose.
Should I stop statins if I have muscle pain?
Don’t stop without talking to your doctor. Muscle pain doesn’t always mean you need to quit. Often, adjusting the dose, switching statins, or trying a different schedule (like every-other-day) helps. Stopping statins increases your heart attack risk-especially if you’ve already had one. Your doctor can check your creatine kinase levels and help you find a solution that protects your heart without hurting your muscles.
Are generic statins as good as brand names?
Yes. Generic statins like atorvastatin, simvastatin, and rosuvastatin are chemically identical to their brand-name versions (Lipitor, Zocor, Crestor). They’re held to the same strict manufacturing standards. The only difference is cost-generics can cost as little as £4 per month in the UK. There’s no reason to pay more unless your doctor has a specific reason to choose a brand.
Can lifestyle changes replace statins?
For some people-especially those with mild cholesterol elevation and no heart disease-lifestyle changes can be enough. Eating more fiber, walking daily, losing weight, and cutting sugar can lower LDL by 10-20%. But if you’ve had a heart attack, stroke, or have diabetes, lifestyle alone usually isn’t enough. Statins reduce risk by 30% or more. That’s a level of protection no diet or exercise program can match. They work best together-not instead of each other.


David Brooks
December 7, 2025 AT 14:36Statins saved my dad’s life after his bypass. He was skeptical too-thought he’d be stuck with leg cramps forever. Switched from simvastatin to pravastatin and now he hikes every weekend. Don’t let fear write your health story. There’s always a version that works.
PS: CoQ10? I started taking it just in case. Feels like a small price to pay for peace of mind. 💪❤️
Jennifer Anderson
December 7, 2025 AT 15:27okay so i was on lipitor for 2 years and my thighs felt like concrete. i thought it was just aging or me being lazy. then i switched to fluvastatin and boom-no more pain. i’m not even kidding. i started walking again. like, actually walking. not just to the fridge.
also-generic is fine. don’t let pharma make you feel guilty for saving $200 a month. 🙃
Sadie Nastor
December 7, 2025 AT 23:26Just wanted to say thank you for writing this. I’ve been terrified of statins since my aunt had that ‘rhabdo’ thing in 2018. But reading how common the muscle pain is actually just placebo or coincidence? That’s a game changer.
I’m 68, prediabetic, LDL at 4.5. My doc said statin. I said no. Now I’m gonna ask about pravastatin. And CoQ10. And maybe… just maybe… give it a shot. 🤞💛
Nicholas Heer
December 9, 2025 AT 22:13Big Pharma’s latest brainwash. Statins? They’re just a cash cow disguised as medicine. You think your doctor cares about your heart? Nah. They get kickbacks. They get bonuses. The real cause of heart disease? Sugar. Processed food. The FDA? Bought and paid for. They don’t want you to know you can fix it with apple cider vinegar and sunlight.
And CoQ10? They don’t sell that. So they ignore it. Wake up, sheeple.
Sangram Lavte
December 11, 2025 AT 03:12As someone from India where statin use is rising fast, I appreciate this breakdown. Many here stop statins because of muscle pain without checking CK levels. The cultural belief is ‘if it hurts, stop it’-but heart disease kills silently here too.
Switching statins works. We’ve seen it in clinics. And yes, generics are perfect. No need for expensive brands. Simple science, not marketing.
Oliver Damon
December 11, 2025 AT 10:47The real insight here isn’t just about statins-it’s about the epistemology of side effects. We conflate correlation with causation constantly in medicine. The placebo-controlled trials showing 70% of ‘statin pain’ occurs on placebo? That’s profound.
It suggests a biopsychosocial model: the body responds not just to molecules, but to narrative. Fear becomes somatic. The drug isn’t the villain-the story around it is. We need more medicine that addresses that.
Wesley Phillips
December 11, 2025 AT 17:01Let’s be real-statins are the only thing keeping the middle class from dying at 55. I mean, look at the data. 30% reduction in heart attacks? That’s not medicine. That’s a miracle. And you’re gonna quit because your legs feel ‘a little heavy’? Bro. You’re not special. You’re just lazy.
CoQ10? Cute. Try not being a hypochondriac for once.
Desmond Khoo
December 12, 2025 AT 16:02My grandma took simvastatin for 10 years. Never had a problem. Then she switched to atorvastatin and started saying her knees felt like they were full of sand. One week later-switched back. All good.
Point is: not all statins are the same. And your doc might not know that. So do your homework. And yes, CoQ10 helped her too. Not magic, but nice. 🌿
Louis Llaine
December 14, 2025 AT 07:45Wow. A 1500-word essay on statins. And still no one mentions the elephant in the room: the pharmaceutical industry makes billions off this. Meanwhile, nobody talks about how diet changes can do 80% of the same work.
Also, ‘muscle pain is just in your head’? That’s what they said about chronic fatigue. And now look where we are.
Pass the popcorn. This is a soap opera.
Jane Quitain
December 15, 2025 AT 05:51YOU CAN DO THIS. I was scared too. But I switched to pravastatin and started walking 20 mins a day. And guess what? I feel stronger than I have in years. Your heart is worth it. You’re worth it. Don’t give up. 💕
Kyle Flores
December 16, 2025 AT 09:49My brother had muscle pain on rosuvastatin. He thought he had to live with it. Then his doctor suggested every-other-day dosing. He’s been on it for 3 years now. No pain. LDL under 2.0.
Don’t assume you’re stuck. There’s a version for you. Just keep talking to your doctor. And don’t let the fear win.
Ryan Sullivan
December 16, 2025 AT 17:17Statins are the most overhyped intervention since low-fat diets. The risk-benefit ratio is a statistical mirage for primary prevention. For someone with no prior CVD, the NNT to prevent one event is over 100. Meanwhile, the number of people who develop myalgia? 1 in 10. That’s not medicine. That’s a numbers game.
And don’t get me started on CoQ10 being ‘worth a shot.’ It’s a placebo with a price tag.
Olivia Hand
December 16, 2025 AT 20:52Why do we assume muscle pain = statin toxicity? What if it’s just inflammation from sitting all day? Or vitamin D deficiency? Or stress? The article mentions SLCO1B1 but ignores the bigger picture: our bodies aren’t broken machines. We’re adaptive systems.
Maybe we need to look beyond the pill. Not to reject it-but to contextualize it.
Stacy here
December 18, 2025 AT 04:18Statins are just the tip of the iceberg. The real agenda? Keep you docile. Keep you dependent. Keep you buying pills instead of fixing your life. The liver doesn’t ‘make cholesterol’-it makes it because you’re eating processed carbs and sitting on your ass.
They don’t want you to know that. They want you to believe a pill can fix what your lifestyle broke.
Wake up. The system is rigged. And your heart? It’s just collateral damage.
Helen Maples
December 19, 2025 AT 15:30As a nurse who’s worked in cardiology for 18 years, I’ve seen patients die because they stopped statins after one bad week of muscle soreness. Please-don’t be one of them.
Switch statins. Lower the dose. Try CoQ10. Try every-other-day. But don’t quit cold turkey. Your heart doesn’t get a second chance.
And if your doctor isn’t listening? Find a new one. You deserve better.