Triple-negative breast cancer doesn’t respond to hormone therapy or HER2-targeted drugs. That’s not a mistake-it’s the definition. About 1 in 10 breast cancer cases are triple-negative, and they’re among the most aggressive. They grow fast, come back quickly, and have fewer treatment options than other types. But the landscape is changing. In 2025 and 2026, new strategies are giving patients more hope than ever before-not just longer survival, but better quality of life during treatment.
Why Triple-Negative Breast Cancer Is So Hard to Treat
Triple-negative breast cancer (TNBC) gets its name because the cancer cells lack three key receptors: estrogen, progesterone, and HER2. That means drugs like tamoxifen or trastuzumab, which work for other breast cancers, simply don’t work here. For years, chemotherapy was the only option. And while chemo can shrink tumors, it’s brutal. Many patients experience severe side effects-fatigue, nerve damage, low blood counts-and still face high chances of the cancer returning within the first three to five years.
What makes TNBC especially tricky is its diversity. Not all TNBC is the same. Some tumors have BRCA gene mutations. Others have high levels of PD-L1, a protein that helps cancer hide from the immune system. Some are packed with mutations that make them visible to the immune system. That’s why a one-size-fits-all approach doesn’t work anymore. Treatment now depends on what’s inside the tumor-not just where it is.
Standard Treatment Today: Chemo, Surgery, and Beyond
For early-stage TNBC, the standard starts with neoadjuvant chemotherapy-chemo before surgery. The goal? Shrink the tumor so surgeons can remove it more easily, and see how well the cancer responds. A complete response-no cancer left in the breast or lymph nodes after chemo-is a strong sign the patient will do well long-term.
The most common chemo combo in the UK and US includes drugs like carboplatin and paclitaxel, sometimes with anthracyclines like doxorubicin. These regimens typically last 18 to 24 weeks. But a new approach from UT Southwestern Medical Center, published in early 2025, is shaking things up. Instead of starting with chemo, they give radiation first, then just two doses of pembrolizumab (an immunotherapy drug), followed by chemo. The result? The same rate of tumor clearance-59%-but with only 41% of patients experiencing serious side effects, compared to 82% in older protocols. That’s a massive drop in toxicity.
After chemo comes surgery, then often more chemo or radiation. But now, for some patients, that’s not the end. If the tumor has high PD-L1 levels, they may get pembrolizumab for a full year after surgery to lower the risk of recurrence. For those with BRCA mutations, PARP inhibitors like olaparib or talazoparib are now part of the standard after surgery.
Immunotherapy: Turning the Body’s Defenses Against Cancer
Immunotherapy isn’t magic, but for the right patients, it’s life-changing. About 40% of metastatic TNBC tumors express PD-L1. That means they’re hiding from immune cells using a protein called PD-L1. Drugs like pembrolizumab and atezolizumab block that signal, letting the immune system see and attack the cancer.
In the KEYNOTE-522 trial, adding pembrolizumab to chemo before surgery boosted the chance of a complete response from 51% to 64.8% in PD-L1-positive patients. In the IMpassion130 trial, atezolizumab plus nab-paclitaxel extended survival by nearly two months in metastatic TNBC. These aren’t small gains-they’re the difference between months and years.
But here’s the catch: if your tumor is PD-L1 negative, immunotherapy adds little benefit. That’s why testing is non-negotiable. Every TNBC patient should have their tumor tested for PD-L1 using the 22C3 pharmDx assay before starting treatment. And it’s not just about one drug. Newer checkpoint inhibitors like durvalumab (Imfinzi®) showed 92.5% three-year survival in the GeparNuevo trial when added to chemo for early-stage TNBC.
Targeted Therapies: Hitting Cancer Where It Hurts
BRCA mutations are present in 15-20% of TNBC cases. These mutations break the cell’s ability to repair DNA damage. PARP inhibitors like olaparib and talazoparib exploit that weakness. In the OlympiAD trial, patients on olaparib lived 7.8 months longer without their cancer worsening compared to those on standard chemo. That’s why BRCA testing is now recommended for every TNBC patient at diagnosis-not just those with family history.
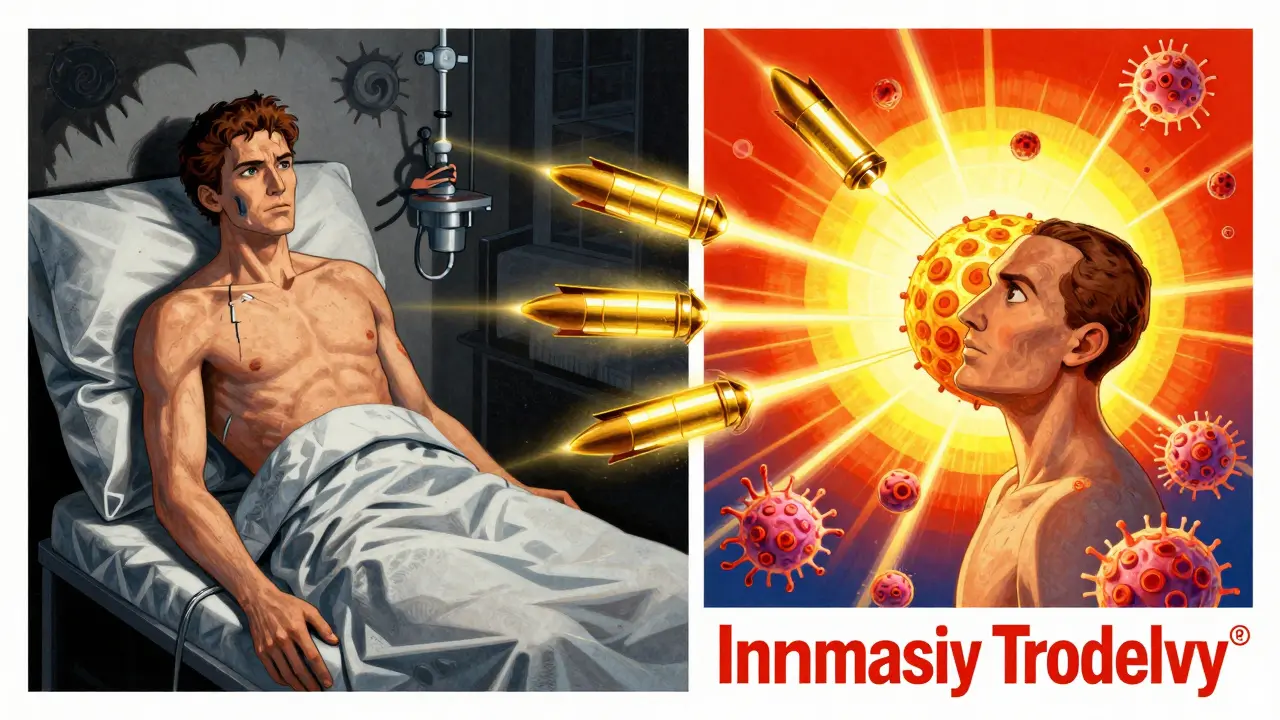
Then there’s sacituzumab govitecan (Trodelvy®), an antibody-drug conjugate. It’s like a smart missile: it homes in on a protein called TROP-2, found on most TNBC cells, and delivers a powerful chemo drug directly inside them. In the ASCENT trial, it cut the risk of death by 57% and the risk of disease progression by 56% compared to chemo. Response rates hit 35%, with median duration of response at 5.6 months. It’s now a standard option after one prior chemo for metastatic TNBC.
Another promising option is trastuzumab deruxtecan (Enhertu®). Even though TNBC is HER2-negative, some tumors have very low levels of HER2. In the DESTINY-Breast04 trial, this drug worked in those patients, with a 37% response rate. It’s not yet approved for TNBC, but many oncologists are using it off-label-and trials are underway to confirm its role.
The New Frontier: Personalized Vaccines and Dual-Target Therapies
The most exciting developments aren’t just drugs-they’re whole new ways of thinking. At Houston Methodist Hospital, researchers are making custom vaccines for each patient. They sequence the tumor’s DNA, find its unique mutations (neoantigens), and build a vaccine in-house within six weeks. Then they pair it with pembrolizumab. In phase I trials, 78% of patients showed strong immune activation. The goal? Not just to treat cancer, but to prevent it from coming back.
Another breakthrough is dual-target therapy. Instead of hitting one pathway, these treatments strike two at once. For example, combining a CDK12 inhibitor with a PARP inhibitor creates synthetic lethality-cancer cells can’t survive the double blow. In lab models, this combo blocked 68% of tumor growth, compared to 32% with PARP alone. Similar strategies are being tested with CDK4/6 and PI3K inhibitors. These aren’t yet standard, but they’re in phase II trials and could reshape treatment in the next two years.
What’s on the Horizon? Trials to Watch in 2025-2026
More than 1,500 clinical trials for TNBC are active worldwide. Here are the most promising ones:
- Datopotamab deruxtecan (Dato-DXd): A new antibody-drug conjugate targeting TROP2. Phase III trials show it outperforms chemo in metastatic TNBC.
- Adagloxad simolenin: A vaccine-like therapy that targets a protein called Globo-H, found on many TNBC cells. Phase III trials are underway.
- CDK12/PARP inhibitor combos: Early results show deep, lasting responses in patients who previously failed other treatments.
- Personalized neoantigen vaccines: Houston Methodist’s approach is expanding to other cancers. If successful, it could become the new standard for preventing recurrence.
The NCCN guidelines are expected to update in May 2026 to include the UT Southwestern protocol and possibly expand immunotherapy use to more patients based on tumor mutational burden.

Challenges and Real-World Barriers
Despite progress, big problems remain. Five-year survival for metastatic TNBC is still only 12-15%, compared to 28% for other breast cancers. Many patients develop resistance. Tumors evolve. New mutations appear. And access is unequal. In low- and middle-income countries, only 35-40% of patients get tested for BRCA or PD-L1. Without testing, they can’t get the right drugs.
Also, these new treatments are expensive. Sacituzumab govitecan costs over $150,000 per year. Immunotherapy can cost even more. Insurance coverage varies. Even in the UK, not all hospitals offer the latest testing or drugs right away. That’s why multidisciplinary tumor boards-teams of oncologists, pathologists, and genetic counselors-are critical. They ensure each patient gets the right test, the right drug, at the right time.
What You Need to Ask Your Doctor
If you or someone you love has TNBC, here are five questions to ask:
- Has my tumor been tested for PD-L1 and BRCA mutations?
- Am I a candidate for immunotherapy or a PARP inhibitor?
- Is there a clinical trial I should consider?
- Can we start with a shorter, less toxic treatment like the UT Southwestern protocol?
- Will my treatment plan include genetic counseling or testing for other family members?
The goal isn’t just to survive. It’s to live well during treatment. And with today’s options, that’s more possible than ever.
Is triple-negative breast cancer curable?
Early-stage triple-negative breast cancer can be cured in many cases, especially if the tumor responds well to chemotherapy and no cancer remains after treatment. About 60-70% of patients with early-stage TNBC who achieve a complete pathologic response after neoadjuvant therapy remain cancer-free at five years. But if the cancer has spread beyond the breast and lymph nodes (metastatic), it’s currently not curable. The goal shifts to controlling the disease, extending life, and maintaining quality of life. New treatments like immunotherapy and antibody-drug conjugates are helping more patients live longer than ever before.
What does PD-L1 positive mean for TNBC treatment?
PD-L1 positive means the cancer cells are using a protein called PD-L1 to hide from your immune system. If your tumor tests positive (CPS ≥10), you’re likely to benefit from immunotherapy drugs like pembrolizumab or atezolizumab. These drugs block PD-L1, letting your immune system attack the cancer. In clinical trials, adding pembrolizumab to chemo improved survival and increased the chance of a complete response by more than 10 percentage points in PD-L1 positive patients. Testing for PD-L1 is now standard before starting treatment.
Are PARP inhibitors only for people with BRCA mutations?
Currently, PARP inhibitors like olaparib and talazoparib are approved for TNBC patients with inherited (germline) BRCA1 or BRCA2 mutations. These mutations impair the cell’s ability to repair DNA, and PARP inhibitors exploit that weakness. While researchers are studying whether patients with other DNA repair defects (like HRD) might also benefit, only those with confirmed BRCA mutations are guaranteed coverage and clinical benefit under current guidelines. All TNBC patients should have BRCA testing at diagnosis, even without a family history.
How does sacituzumab govitecan work?
Sacituzumab govitecan (Trodelvy®) is an antibody-drug conjugate. It has two parts: an antibody that sticks to TROP-2, a protein found on most TNBC cells, and a powerful chemotherapy drug attached to it. Once the antibody finds the cancer cell, it delivers the chemo directly inside, killing the cell while sparing healthy ones. In the ASCENT trial, it reduced the risk of death by 57% compared to standard chemo in patients who had already tried at least two prior treatments. Side effects include low white blood cell counts and diarrhea, but they’re often manageable with support.
Can I get a personalized vaccine for TNBC?
Personalized neoantigen vaccines are still experimental and only available through clinical trials. As of 2025, Houston Methodist Hospital is one of the few centers offering this in phase I trials. The vaccine is made from your own tumor’s DNA and takes about six weeks to produce. It’s given with pembrolizumab to boost the immune response. While early results are promising-with 78% of patients showing strong immune activation-it’s not yet standard care. If you’re interested, ask your oncologist if you qualify for a trial or if any are open near you.
Next Steps: What to Do Now
If you’ve been diagnosed with TNBC, start with three things:
- Get full biomarker testing: PD-L1, BRCA1/2, and ideally, a broader genomic panel for HRD and tumor mutational burden.
- Ask about clinical trials. Many of the most effective new treatments are only available through trials right now.
- Seek care at a center with a multidisciplinary tumor board. TNBC is complex. You need experts in oncology, pathology, genetics, and radiation working together.
The future of TNBC treatment isn’t about stronger chemo. It’s about smarter, targeted, personalized care. The tools are here. The science is advancing fast. And for the first time, patients have real options beyond the old standard of ‘just endure chemo and hope for the best.’


Hannah Gliane
February 2, 2026 AT 04:21Sandeep Kumar
February 2, 2026 AT 08:53Gary Mitts
February 2, 2026 AT 10:36Becky M.
February 3, 2026 AT 00:00Bob Hynes
February 4, 2026 AT 05:26Eli Kiseop
February 5, 2026 AT 00:42Akhona Myeki
February 6, 2026 AT 06:49Chinmoy Kumar
February 7, 2026 AT 20:09