Every year in the U.S., over 1.5 million people end up in the emergency room because of problems with their medications. That’s not just a statistic-it’s your neighbor, your parent, your friend. Many of these cases aren’t accidents. They’re preventable. This is where medication safety comes in-not as a fancy hospital policy, but as a basic right you deserve when you take a pill, use an inhaler, or get an injection.
What Exactly Is Medication Safety?
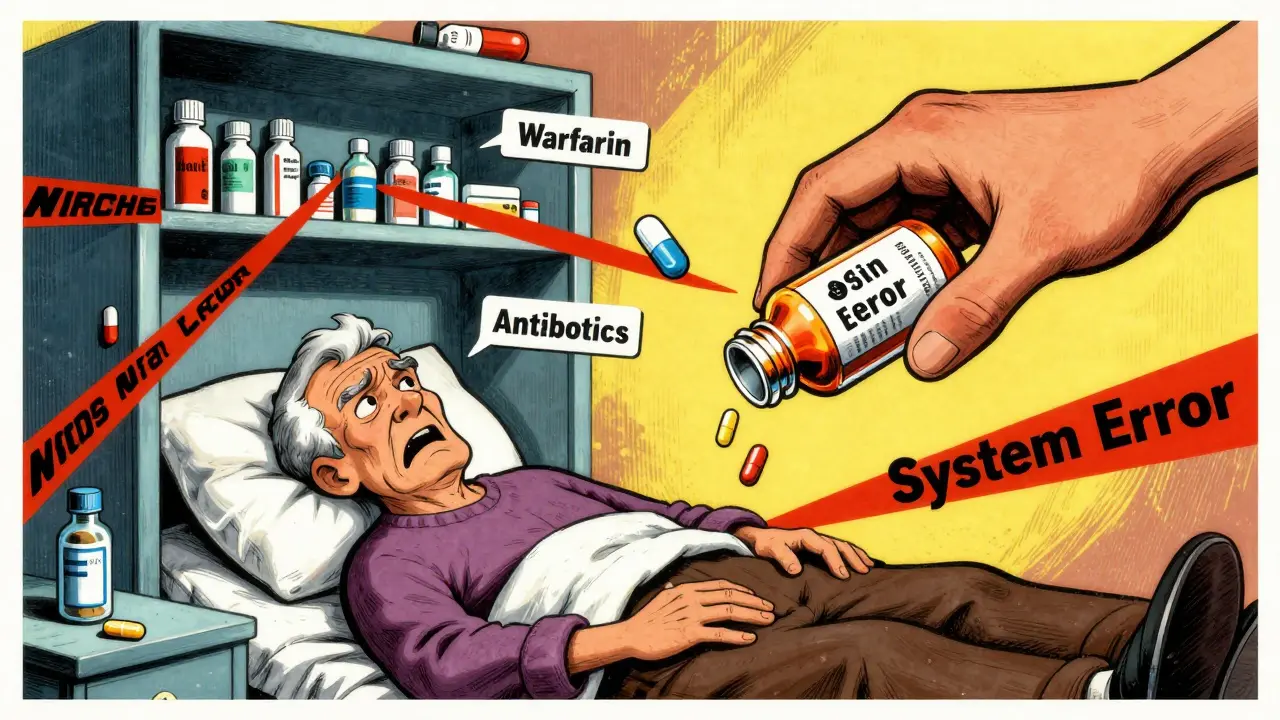
Medication safety isn’t just about doctors writing clear prescriptions. It’s the entire system that keeps you from being harmed by the very drugs meant to help you. The National Patient Safety Foundation defines it simply: freedom from accidental injury due to errors in the medication-use process. That process? It’s longer than you think. It starts when a drug is ordered, goes through storage, labeling, dispensing, and finally reaches you-and then continues with how you take it, what you tell your doctor, and whether your pills are monitored properly. There are nine stages in this process. At each one, something can go wrong. Prescribing errors make up 38% of all mistakes. That’s when a doctor writes the wrong dose, picks the wrong drug, or doesn’t check for interactions. Administration errors-like a nurse giving the wrong pill at the wrong time-account for another 26%. And let’s not forget the patient: skipping doses, mixing pills with alcohol, or taking leftover antibiotics because they "felt better" are all part of the picture. The goal isn’t just to avoid mistakes. It’s to make sure you get the right drug, in the right amount, at the right time, for the right reason. And if something goes wrong, the system catches it before you do.Why Medication Errors Happen-And Who’s Most at Risk
You might think errors only happen in busy hospitals. But they happen everywhere. A 78-year-old woman takes her blood pressure pill and her diabetes pill together because they look similar. A child gets 10 times the correct dose because a liquid medication was measured with a kitchen spoon instead of a syringe. A young adult skips their antidepressant for a week because they can’t afford it, then restarts and feels worse. Certain groups are far more vulnerable. People over 65 make up half of all hospitalizations due to medication problems. Kids under 12 account for 20% of emergency visits from adverse drug events. Pregnant women face unique risks-some medications can harm a developing baby even at low doses. And patients on five or more medications? They’re at 35% higher risk of an error. That’s called polypharmacy, and it’s becoming more common as people live longer with multiple chronic conditions. High-alert medications are especially dangerous. Insulin, opioids, blood thinners like warfarin, and IV oxytocin (used during labor) are on the list for a reason. One wrong dose can lead to coma, internal bleeding, or death. In fact, insulin alone is involved in 17% of serious medication errors.How Technology Is Making Medication Safety Better
Technology isn’t perfect-but it’s saving lives. Electronic health records (EHRs) with built-in safety checks have cut serious medication errors by nearly half in hospitals. Barcode scanning at the bedside? That’s reduced administration errors by 65%. When a nurse scans your wristband and the pill bottle, the system checks: Is this the right drug? The right dose? The right time? If not, it stops them. The FDA’s 2023 rule requiring standardized numeric dosing on all prescription labels has already reduced decimal point errors by 32%. No more ".5 mg" that could be misread as "5 mg." Now it’s clearly written as "0.5 mg"-a tiny change, but a huge safety win. Even pharmacies are stepping up. Blister packs that organize pills by day and time have improved adherence by 60% in older adults. And apps that send reminders or flag potential drug interactions? They’re not magic-but they help.What You Can Do Right Now to Protect Yourself
You don’t have to wait for hospitals or pharmacies to fix everything. You have power too.- Keep an updated list of every medication you take-including over-the-counter pills, vitamins, and herbal supplements. Include the dose and why you take it. Use the CDC’s free template. Bring it to every appointment.
- Ask three questions every time you get a new prescription: What is this for? How do I take it? What side effects should I watch for? Don’t be shy. A 2022 study found patients who asked these questions were 40% less likely to have an error.
- Never guess. If a pill looks different than usual, ask the pharmacist. If the dose seems too high or too low, double-check. A nurse in a Reddit thread said she caught 50 errors in two years just by asking, "Does this make sense?"
- Use a pill organizer if you take multiple meds daily. Even a simple weekly box helps prevent double-dosing or skipping days.
- Don’t stop or change meds because of cost or side effects. Talk to your doctor. There are often cheaper alternatives or ways to manage side effects.
One patient told the CDC she used to mix up her blood thinner and her cholesterol pill because the bottles looked alike. After switching to a pharmacy-provided blister pack, she had zero errors for over a year.
The Bigger Picture: Why This Matters Beyond the Hospital
Medication safety isn’t just about avoiding harm. It’s about getting the best care possible. When systems work, patients recover faster, spend less time in the hospital, and live longer. The CDC estimates that 400,000 preventable injuries happen in U.S. hospitals each year because of medication errors. That’s 1,100 a day. And it costs the system $42 billion annually. But here’s the good news: comprehensive safety programs can cut those errors by 50% to 80%. Hospitals that follow the "Five Rights"-right patient, right drug, right dose, right route, right time-plus three more: right documentation, right reason, and right response-see dramatic drops in harm. The World Health Organization’s "Medication Without Harm" campaign has already helped countries reduce severe medication-related harm by 15% to 25% in just two years. The U.S. is slowly catching up, but progress is uneven. Only 55% of hospitals have full clinical decision support systems. Many still rely on handwritten notes or rushed verbal orders.What’s Holding Us Back?
It’s not lack of knowledge. It’s culture. For years, when a mistake happened, the focus was on punishing the person who made it-the nurse, the pharmacist, the doctor. But research shows that 80% of errors come from flawed systems, not careless people. The Institute for Healthcare Improvement found that only 35% of healthcare organizations have true non-punitive reporting systems. That means if you report an error, you’re more likely to get in trouble than to get help fixing the system. Another problem? Alert fatigue. Clinical decision systems can flood providers with 25+ alerts per patient. After a while, they start ignoring them-even the important ones. And then there’s cost. Installing a full safety system in a 100-bed hospital can cost $250,000. But the return? Every dollar spent saves $4.20 in avoided hospital stays, lawsuits, and long-term care.
The Future of Medication Safety
The future is smarter. AI tools are being tested to scan your EHR and predict which medication combo might cause a dangerous interaction-even before your doctor prescribes it. In pilot programs, this has cut potential adverse events by 40%. Blockchain is being used in Europe to track pills from manufacturer to pharmacy, cutting counterfeit drugs by 65%. Telehealth, while convenient, has led to a 300% spike in medication errors since 2022-mostly because doctors can’t see patients or check their pill bottles during virtual visits. Personalized medicine is growing fast. But with it comes complexity. A single cancer patient might be on 10+ drugs, each with unique timing, food restrictions, and monitoring needs. That’s where medication safety becomes even more critical.You’re Not Just a Patient. You’re a Partner.
Medication safety isn’t something that happens to you. It’s something you help build. Whether you’re taking one pill a day or ten, you have the right to understand what you’re taking and why. You have the right to ask questions. You have the right to speak up when something doesn’t feel right. The system isn’t perfect. But it’s getting better. And you’re part of that change.What’s the difference between a medication error and an adverse drug event?
A medication error is a mistake that happens during prescribing, dispensing, or taking a drug-like getting the wrong dose or mixing two pills that shouldn’t be taken together. An adverse drug event (ADE) is the actual harm that results-like a fall from low blood pressure, liver damage from a reaction, or a hospital stay. Not all errors cause harm, but all ADEs start with an error. The goal of medication safety is to stop the error before it becomes an event.
Can I trust my pharmacist to catch medication errors?
Pharmacists are trained to catch errors, and most do. But they’re also busy. A single pharmacist might fill 200+ prescriptions in a day. That’s why it’s critical you double-check your meds too. If a pill looks different, if the instructions seem odd, or if you’ve never taken it before-ask. Say: "This isn’t what I usually get. Can you confirm this is right?"
Why do some medications have black box warnings?
Black box warnings are the strongest safety alert the FDA can require. They’re used for drugs that carry serious, even life-threatening risks-like heart failure, severe allergic reactions, or increased suicide risk. These aren’t rare side effects. They’re known dangers that require extra caution. If your prescription has one, ask your doctor: "What signs should I watch for? What should I do if I notice them?"
Is it safe to take herbal supplements with my prescription drugs?
Not always. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can increase bleeding risk, especially before surgery. Grapefruit juice can dangerously boost levels of some statins and blood pressure meds. Always tell your doctor and pharmacist about every supplement you take-even if you think it’s "natural" or "harmless."
What should I do if I think I’ve had a medication error?
If you notice something wrong-like unusual drowsiness, rash, confusion, or a sudden change in how you feel-contact your doctor or pharmacist immediately. Don’t wait. If it’s an emergency, go to the ER. Then report it. You can file a report with the FDA’s MedWatch program or your local hospital’s safety office. Reporting helps fix systems so others don’t get hurt.
Are there free tools to help me manage my medications?
Yes. The CDC offers a free printable medication list template you can fill out and bring to appointments. Many pharmacies offer free blister packs for chronic meds. Apps like Medisafe and MyTherapy send reminders and track interactions. AARP also has a free Medication Safety Toolkit with checklists and conversation starters for talking to your doctor.

Melissa Taylor
December 16, 2025 AT 01:53Medication safety isn’t glamorous, but it’s the quiet hero of everyday healthcare. I’ve seen my mom nearly take two blood pressure pills because the bottles looked identical. A simple blister pack changed everything. No drama, no panic-just a system that works. We don’t need grand gestures. We need consistent, simple protections for everyone, especially the elderly and those juggling five meds at once.
John Brown
December 17, 2025 AT 22:23Real talk-most people don’t know half of what they’re taking. I used to just swallow whatever the doc handed me until my cousin ended up in the ER from mixing OTC painkillers with her antidepressant. Now I ask the three questions every time. Turns out, pharmacists appreciate it. They’re not robots, they’re people trying to keep up. A little effort on our end saves lives. And yeah, I use a pill organizer. No shame in it.
Sai Nguyen
December 18, 2025 AT 12:20America’s healthcare system is a joke. You need a PhD just to take a pill. Why is this even a conversation? In my country, doctors prescribe, patients obey. No apps. No lists. No confusion. This overcomplication is why your system fails.
Benjamin Glover
December 19, 2025 AT 06:09How quaint. A 2023 FDA labeling rule is hailed as a breakthrough? We’ve had standardized dosing in the UK for decades. And yet, here you are, applauding basic hygiene. The real issue isn’t technology-it’s the cultural tolerance for mediocrity in clinical practice. You don’t need apps. You need accountability.
Raj Kumar
December 20, 2025 AT 07:43Been there. My aunt was on 8 meds, and the pharmacy gave her a pillbox with no labels. She mixed up the anticoagulant with the thyroid med. Scary stuff. But once we got the free AARP toolkit, started using Medisafe, and sat down with her pharmacist-everything clicked. It’s not about being perfect. It’s about being consistent. And yeah, sometimes the system fails, but the tools are there. Use ‘em.
Jocelyn Lachapelle
December 21, 2025 AT 20:02My grandma took her meds like clockwork-until she started forgetting which was which. Then we switched to the pharmacy’s blister packs. No more guessing. No more panic. She even started smiling when she opened her weekly box. Simple fixes work. You don’t need AI or blockchain. You need someone who cares enough to help you organize. That’s the real tech.
Mike Nordby
December 22, 2025 AT 10:12It’s worth noting that while technology reduces errors, it also introduces new failure modes-alert fatigue, interface design flaws, and interoperability gaps between EHR systems. The 65% reduction in administration errors via barcode scanning is impressive, but only if the barcode is correctly printed, the scanner is calibrated, and the nurse isn’t overwhelmed by 27 alerts per patient. Human factors engineering remains the missing piece. Systems must adapt to users, not the reverse.
John Samuel
December 22, 2025 AT 13:01Let’s be real-medication safety isn’t just about pills and protocols. It’s about dignity. It’s about a 78-year-old woman not having to squint at tiny labels. It’s about a single mom choosing between rent and her insulin. It’s about a kid getting the right dose because someone didn’t use a kitchen spoon. This isn’t healthcare bureaucracy. This is human survival. And if we can’t get this right, what the hell are we even doing?